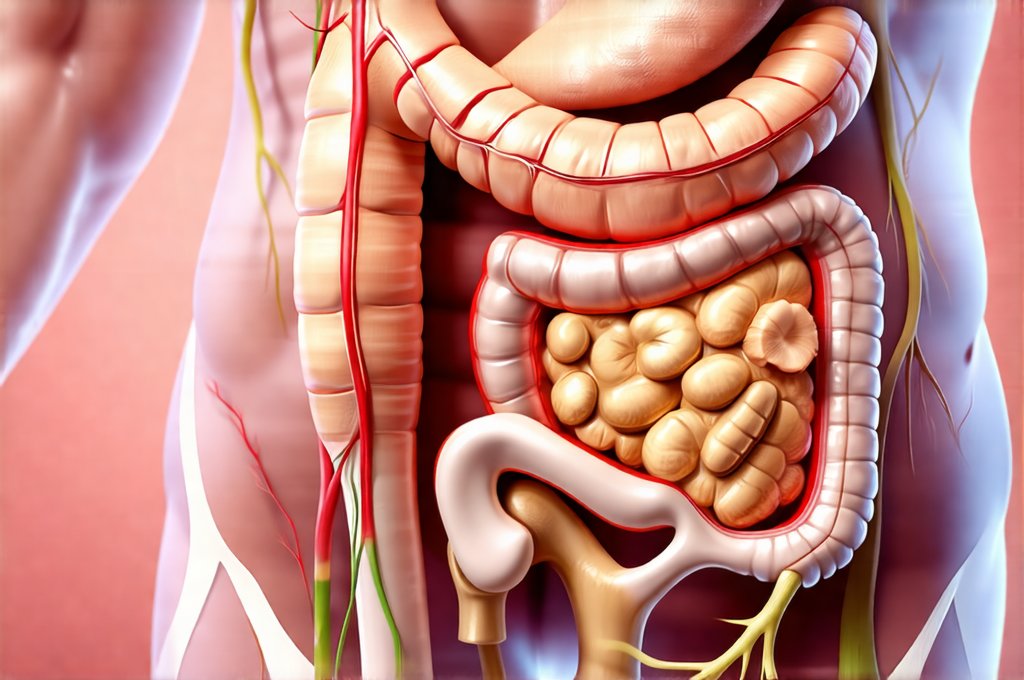
Irritable Bowel Syndrome (IBS) is a frustrating condition impacting millions worldwide, characterized by abdominal pain, bloating, gas, diarrhea, and/or constipation. It’s often a diagnosis of exclusion – meaning other potential causes are ruled out first – because its symptoms overlap with so many other conditions. Beyond the digestive discomfort, there’s growing recognition that IBS isn’t just a gut problem; it frequently co-exists with systemic inflammation, nutrient deficiencies, and even compromised bone health. This is due to several factors including malabsorption issues common in IBS, chronic stress responses impacting vitamin D activation, and potential dietary restrictions inadvertently limiting essential nutrients needed for strong bones. Addressing IBS effectively therefore requires a holistic approach, one that simultaneously soothes the gut and supports long-term skeletal integrity.
Many conventional treatments focus on symptom management – antispasmodics, laxatives, anti-diarrheals – but these often don’t address the underlying causes or prevent future issues. Furthermore, they can sometimes disrupt the delicate balance of the gut microbiome even further. A truly effective IBS plan prioritizes healing the gut lining, restoring microbial diversity, managing stress, and ensuring adequate nutrient intake for optimal bone health. This isn’t about quick fixes; it’s about building a foundation of wellness that supports both digestive comfort and structural strength over the long term. It is vital to work with qualified healthcare professionals – doctors, registered dietitians specializing in gut health, and potentially physical therapists – to develop an individualized plan. Considering a meal plan could be a good starting point.
Gut-Healing Foundations for IBS & Bone Health
A cornerstone of any effective IBS management strategy is addressing gut permeability, often referred to as “leaky gut.” This occurs when the tight junctions between cells lining the intestinal wall become compromised, allowing undigested food particles, bacteria, and toxins to enter the bloodstream. This triggers an immune response, leading to inflammation that can contribute to both digestive symptoms and systemic issues like bone loss. Restoring the integrity of the gut barrier is therefore paramount. Dietary interventions play a huge role here. – Reducing inflammatory foods such as processed sugars, refined carbohydrates, excessive alcohol, and artificial sweeteners – all known irritants for IBS sufferers. – Incorporating easily digestible protein sources like fish, poultry (skinless), and plant-based proteins. – Prioritizing gut-healing nutrients like L-glutamine, collagen peptides, and zinc which support intestinal repair.
Furthermore, the microbiome—the trillions of bacteria residing in our gut—plays a critical role in both digestion and overall health. An imbalance in gut flora (dysbiosis) is often present in IBS sufferers and can exacerbate symptoms. Probiotic supplementation, specifically strains tailored to your individual needs (guided by a healthcare professional), can help restore microbial balance. However, probiotics are not one-size-fits-all. Prebiotics – the food that feeds beneficial bacteria – are equally important. Sources of prebiotics include garlic, onions, leeks, asparagus, bananas, and oats. A diverse diet rich in fiber (introduced gradually to avoid exacerbating symptoms) supports a thriving microbiome. You might find support with a meal plan with digestive enzymes
Finally, managing stress is essential. The gut-brain axis is a bidirectional communication system linking the digestive tract with the central nervous system. Chronic stress can negatively impact gut motility, increase intestinal permeability, and disrupt microbial balance. Practices like mindfulness meditation, yoga, deep breathing exercises, or even spending time in nature can help mitigate the effects of stress on your gut – and subsequently, your overall health.
Nutrient Deficiencies & Bone Density in IBS
IBS often leads to nutrient deficiencies due to malabsorption issues and/or restrictive diets adopted to manage symptoms. Common culprits include vitamin D, calcium, magnesium, iron, folate, and B12. These nutrients are all crucial for bone health. Vitamin D is essential for calcium absorption; without enough vitamin D, your body can’t effectively utilize the calcium you consume. Magnesium plays a role in bone formation and mineralization. Iron deficiency anemia can lead to reduced bone density. A lack of folate and B12 can impact collagen synthesis, which is vital for bone matrix structure. Identifying and addressing these deficiencies through dietary changes or targeted supplementation (under medical supervision) is paramount for protecting bone health.
Regular screening for nutrient deficiencies is recommended for individuals with IBS. Blood tests can help identify specific shortages. Dietary adjustments may involve focusing on foods rich in the deficient nutrients, but absorption issues might necessitate supplemental support. For instance, if calcium absorption is poor, a more bioavailable form like calcium citrate may be preferable to calcium carbonate. It’s also important to consider that certain medications used to manage IBS symptoms can interfere with nutrient absorption, necessitating adjustments to dosage or alternative therapies. A balanced eating plan may help address these deficiencies.
It’s not always about increasing intake, but ensuring proper absorption. Addressing inflammation in the gut is often key to improving nutrient uptake. A healed gut barrier allows for better absorption of nutrients from food and supplements alike. Furthermore, working with a registered dietitian can help you design an individualized meal plan that minimizes trigger foods while maximizing nutrient density – even within dietary restrictions imposed by IBS.
Bone-Boosting Foods & Lifestyle Factors
Beyond addressing deficiencies, proactively incorporating bone-boosting foods into your diet is beneficial. – Leafy green vegetables (kale, spinach, collard greens) are excellent sources of calcium and vitamin K, both essential for bone health. – Fatty fish (salmon, mackerel, sardines) provide vitamin D and omega-3 fatty acids, which have anti-inflammatory properties. – Dairy products (if tolerated) are a good source of calcium and protein. Alternatives like fortified plant milks can also be used. – Weight-bearing exercise is crucial for stimulating bone formation. Activities like walking, running, dancing, and strength training all contribute to stronger bones.
Resistance training – lifting weights or using resistance bands – is particularly effective at increasing bone density. It places stress on the bones, prompting them to become denser and stronger. Even simple bodyweight exercises can be beneficial. Aim for at least 30 minutes of moderate-intensity weight-bearing exercise most days of the week. However, it’s important to listen to your body and avoid overexertion, especially if you’re experiencing IBS symptoms. Consider a daily plan with warm grains for sustained energy levels.
Finally, maintaining a healthy weight is vital. Being underweight or significantly overweight can both negatively impact bone health. Adequate protein intake is also essential for muscle mass and bone density. Aim for 0.8-1 gram of protein per kilogram of body weight daily. Remember that this information isn’t intended to replace professional medical advice; it’s designed to provide a starting point for discussion with your healthcare team.