Irritable Bowel Syndrome (IBS) impacts millions worldwide, often presenting as a frustrating cycle of abdominal pain, bloating, gas, diarrhea, and/or constipation. While there’s no one-size-fits-all cure, dietary modification consistently emerges as a cornerstone of symptom management. Many individuals find significant relief by understanding how different foods interact with their digestive system and proactively building meals that minimize triggers. It’s important to remember that IBS is highly individual; what bothers one person may not affect another, making personalized experimentation key. This article aims to provide practical guidance on constructing balanced plates specifically designed to soothe IBS symptoms and improve overall digestive well-being, moving beyond restrictive diets toward nourishing choices.
Navigating the world of “IBS-friendly” eating can feel overwhelming, with conflicting information abounding. The goal isn’t necessarily about eliminating entire food groups (unless a specific allergy or intolerance exists), but rather understanding how to combine foods and manage portion sizes to reduce digestive stress. This involves recognizing potential trigger foods – often categorized as FODMAPs which we will discuss further – and strategically building meals that prioritize gut health. It’s also vital to work collaboratively with healthcare professionals, such as registered dietitians specializing in IBS, to create a plan tailored to your unique needs and symptoms. A balanced plate isn’t about deprivation; it’s about empowerment through informed food choices.
Understanding the FODMAP Landscape
FODMAPs – Fermentable Oligosaccharides, Disaccharides, Monosaccharides And Polyols – are short-chain carbohydrates that can be poorly absorbed in the small intestine. When these sugars reach the large intestine, they’re fermented by gut bacteria, producing gas and potentially triggering IBS symptoms like bloating, pain, and altered bowel habits. It’s crucial to understand that FODMAPs aren’t inherently bad; they are a natural part of many healthy foods. The issue arises when someone with IBS has difficulty digesting them, leading to an overgrowth of gut bacteria and subsequent discomfort.
The low-FODMAP diet plan PDF isn’t meant to be a long-term solution for everyone, but rather a diagnostic tool. Many people use it as an elimination diet – removing high-FODMAP foods for a period (typically 2–6 weeks) to identify sensitivities, then gradually reintroducing them one by one under the guidance of a healthcare professional. This process helps pinpoint specific triggers and determine what level of tolerance exists. Common high-FODMAP foods include:
- Onions and garlic
- Apples, pears, mangoes
- Wheat and rye (in large quantities)
- Dairy products containing lactose
- Legumes like beans and lentils
- Honey and high-fructose corn syrup
It’s important to note that portion size matters. Some FODMAP foods can be tolerated in small amounts. For example, a small banana might not cause issues, while an entire one could trigger symptoms.
This approach emphasizes mindful eating and understanding your body’s individual response to different foods. A registered dietitian specializing in IBS can provide invaluable support throughout the elimination and reintroduction phases, ensuring nutritional adequacy and preventing unnecessary restriction. The ultimate aim is to create a sustainable, personalized diet that minimizes symptoms while still enjoying a wide variety of nourishing foods.
Building Your Balanced Plate: Practical Strategies
Constructing an IBS-friendly plate begins with understanding key principles. First, prioritize whole, unprocessed foods whenever possible. These tend to be lower in FODMAPs and easier for the digestive system to handle. Second, focus on adequate fiber intake – but choose low-FODMAP sources (more on this below). Fiber is essential for gut health and regularity, but certain types can exacerbate IBS symptoms. Third, manage portion sizes, paying attention to how different foods affect your individual tolerance levels. Fourth, stay hydrated by drinking plenty of water throughout the day, aiding digestion and preventing constipation.
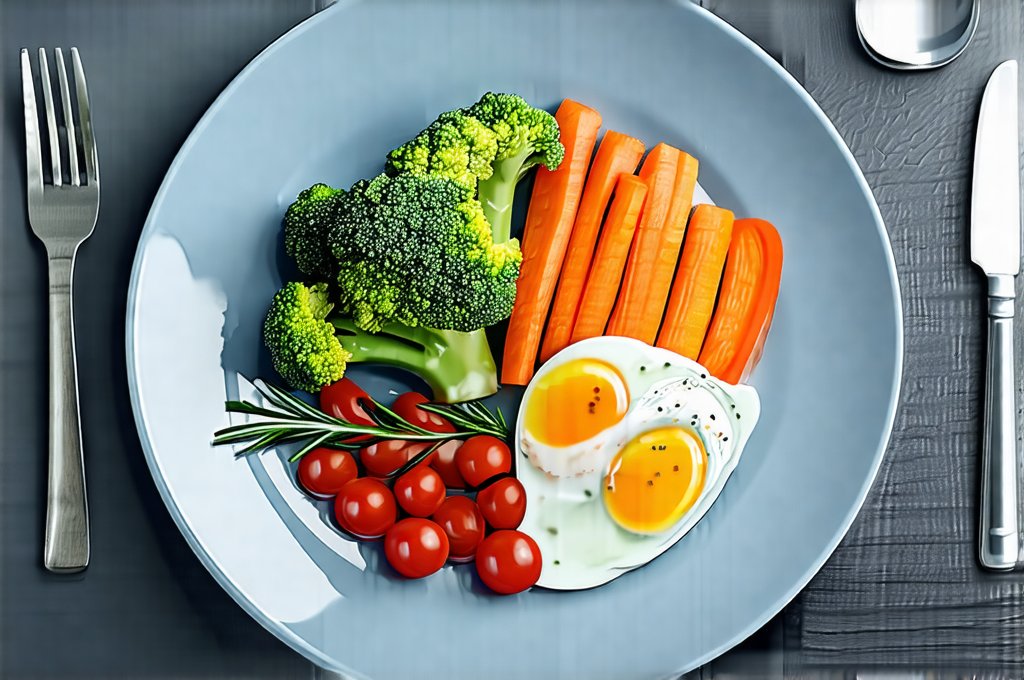
A visually balanced plate should ideally include:
- Approximately 50% non-starchy vegetables: These provide essential vitamins, minerals, and fiber without being overly fermentable. Examples include carrots, spinach, zucchini, bell peppers, and cucumber.
- Approximately 25% lean protein: Protein is vital for overall health and helps stabilize blood sugar levels. Opt for sources like chicken breast, fish, tofu, or eggs.
- Approximately 25% low-FODMAP carbohydrates: Choose options such as quinoa, rice, oats (in moderation), potatoes, or lactose-free dairy alternatives.
Remember to incorporate healthy fats in small amounts – olive oil, avocado, nuts and seeds (again, mindful of portion sizes) – for added nutrients and satiety. Regularly assessing how food combinations impact your symptoms is critical to refining the plate over time. Those looking for relief may find best smoothies helpful as well.
Fiber: Friend or Foe?
Fiber plays a complex role in IBS management. While often recommended for digestive health, not all fiber is created equal. Insoluble fiber, found in wheat bran and some vegetables, can exacerbate symptoms in individuals with IBS due to its bulk-forming properties. Soluble fiber, on the other hand, dissolves in water, forming a gel-like substance that softens stool and promotes regularity. Good sources of low-FODMAP soluble fiber include oats (in moderation), psyllium husk (used cautiously and with plenty of water), carrots, and bananas (ripe ones are lower FODMAP).
It’s crucial to increase fiber intake gradually to avoid sudden digestive upset. Start with small amounts and monitor your body’s response. If you experience increased bloating or gas, reduce the amount of fiber consumed and consider switching to a different source. Experimenting with both soluble and insoluble fibers under professional guidance can help determine what works best for your specific needs. Remember that hydration is key when increasing fiber intake; water helps move fiber through the digestive system and prevents constipation.
Hydration & Gut Health Connection
Staying adequately hydrated is often overlooked, yet it’s profoundly important for IBS management. Water aids in digestion, softens stool, and helps prevent both diarrhea and constipation – two common IBS symptoms. Dehydration can worsen bloating, fatigue, and overall discomfort. Aim for at least eight glasses of water per day, adjusting based on activity level and climate.
Beyond plain water, consider incorporating herbal teas (ginger and peppermint are known to soothe digestion), diluted fruit juices (low-FODMAP options only), or infused water with cucumber and mint. Avoid sugary drinks and excessive caffeine, as these can irritate the digestive system. Pay attention to your body’s signals – thirst is often a late indicator of dehydration. Proactive hydration is a simple but powerful tool for managing IBS symptoms and supporting overall gut health. It’s also important to note that fiber absorbs water, so increasing fiber intake necessitates increased fluid consumption.
Mindful Eating & Symptom Tracking
Building a balanced plate isn’t just about what you eat; it’s also about how you eat. Practicing mindful eating – paying attention to your body’s hunger and fullness cues, chewing thoroughly, and eating slowly – can significantly improve digestion and reduce symptoms. Stress and anxiety often exacerbate IBS, so creating a calm and relaxed mealtime environment is essential.
Furthermore, keeping a food diary or symptom tracker can be incredibly helpful in identifying trigger foods and patterns. Record what you eat, when you eat it, and any associated symptoms (pain, bloating, gas, bowel habits). This information will help you refine your diet and understand your individual sensitivities. There are many apps available to assist with this process, making tracking more convenient. Consistency is key – the more detailed and accurate your records, the better equipped you’ll be to manage your IBS effectively. Remember that working with a registered dietitian can provide personalized guidance on mindful eating techniques and symptom tracking strategies. Implementing a simple clean day once a week could also aid in the process.