The human circulatory system is an astonishing network responsible for delivering oxygen and nutrients to every cell in our bodies while simultaneously removing waste products. When this intricate system falters – whether through poor lifestyle choices, underlying conditions, or simply the aging process – it can lead to a cascade of health problems ranging from fatigue and cognitive decline to serious cardiovascular events. Improving blood flow isn’t merely about athletic performance; it’s fundamental to overall vitality and well-being. Many strategies exist for supporting healthy circulation, including regular exercise, a balanced diet, stress management, and adequate hydration. Increasingly, intermittent fasting (IF) is being recognized as another potentially powerful tool in this arsenal, offering a unique approach to optimizing vascular health through metabolic shifts and cellular repair mechanisms.
Intermittent fasting isn’t a new concept; variations have been practiced for centuries across different cultures, often for religious or spiritual reasons. However, its recent surge in popularity stems from growing scientific interest in its potential benefits beyond weight management. While IF is not a magic bullet and requires careful consideration and potentially professional guidance, the emerging evidence suggests it can influence several key factors that directly impact blood flow and circulatory function. This article will delve into the ways intermittent fasting might contribute to improved circulation, exploring the underlying mechanisms, practical considerations, and potential benefits for overall health. It’s crucial to remember that this information is not a substitute for professional medical advice; always consult with your healthcare provider before making significant changes to your diet or lifestyle.
The Science Behind Intermittent Fasting & Circulation
Intermittent fasting operates on the principle of cycling between periods of eating and voluntary fasting. This isn’t about restricting what you eat, but rather when you eat. Several different methods exist, including:
– Time-Restricted Eating (TRE): Consuming all calories within a specific window each day (e.g., 16/8 method – fasting for 16 hours and eating within an 8-hour window).
– Alternate Day Fasting (ADF): Alternating between days of normal eating and days with very limited calorie intake.
– 5:2 Diet: Eating normally for five days a week and restricting calories on two non-consecutive days.
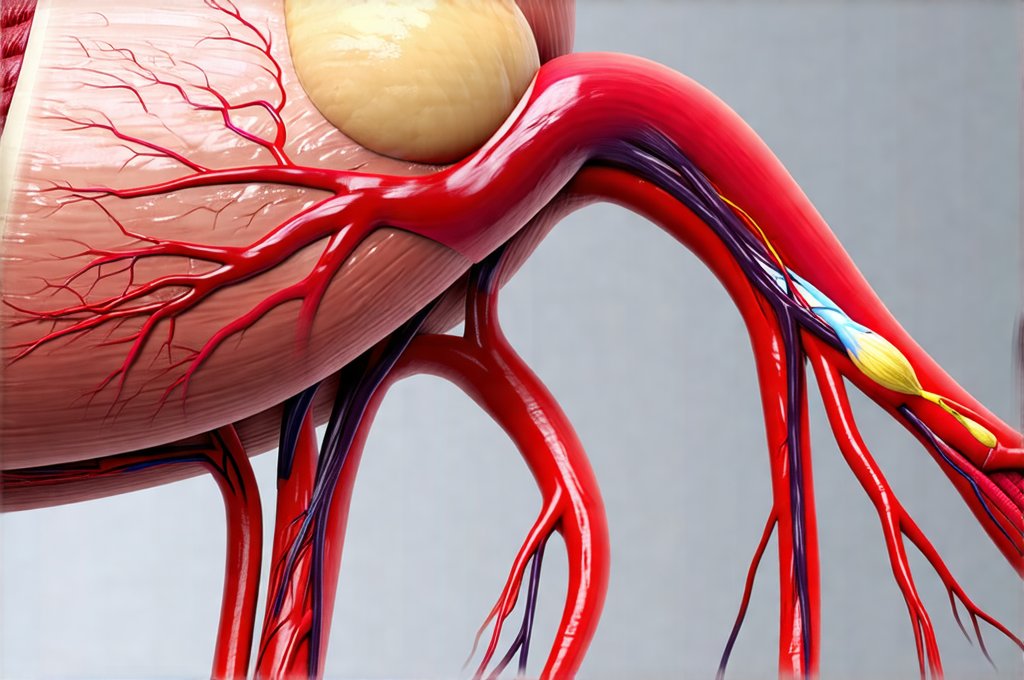
The benefits to circulation appear to stem from several interconnected physiological changes initiated during the fasting period. One key mechanism is improved endothelial function. The endothelium is the inner lining of blood vessels, playing a critical role in regulating blood pressure, preventing clot formation, and maintaining vascular tone. Chronic inflammation can damage the endothelium, leading to impaired function and increased risk of cardiovascular disease. Intermittent fasting has been shown to reduce markers of systemic inflammation, potentially protecting and restoring endothelial health.
Furthermore, IF can positively influence lipid profiles – specifically, it may help lower LDL (“bad”) cholesterol and triglycerides while increasing HDL (“good”) cholesterol. High levels of LDL cholesterol contribute to the buildup of plaque in arteries (atherosclerosis), restricting blood flow. By improving lipid metabolism, intermittent fasting may reduce this risk. The metabolic switch that occurs during fasting—shifting from glucose as the primary fuel source to fatty acids and ketones—also appears to play a role. Ketones, produced when the body breaks down fat for energy, have demonstrated protective effects on vascular cells in some studies. Understanding Does Intermittent Fasting Improve Cholesterol Levels? can help you make informed choices about your health.
Cellular Repair & Vascular Health
A compelling aspect of intermittent fasting’s potential circulatory benefits lies in its ability to stimulate autophagy. Autophagy is essentially the body’s cellular “housekeeping” process – a mechanism where damaged or dysfunctional cells and cell components are removed, allowing for renewal and regeneration. This process is crucial for maintaining healthy tissues and preventing disease. During prolonged periods of fasting (even those within typical IF protocols), cells experience stress which triggers autophagy. This clearing out of cellular debris can improve overall cellular function, including the health of endothelial cells lining blood vessels.
Beyond autophagy, intermittent fasting promotes biogenesis – the creation of new mitochondria within cells. Mitochondria are the powerhouses of our cells, responsible for generating energy. Healthy, abundant mitochondria are essential for proper cell functioning and reduced oxidative stress. Oxidative stress damages cells and contributes to inflammation; therefore, increased mitochondrial biogenesis supports vascular health by reducing damage and enhancing cellular resilience.
The reduction in insulin resistance is another significant benefit. Chronic high insulin levels can contribute to endothelial dysfunction and increase the risk of atherosclerosis. Intermittent fasting helps improve insulin sensitivity, meaning the body requires less insulin to regulate blood sugar, potentially mitigating these risks. This doesn’t just impact cardiovascular health; it’s also linked to improved metabolic function overall. For those managing diabetes, exploring How to Eat for Diabetes With Intermittent Fasting could be a game changer.
Implementing Intermittent Fasting Safely
Before embarking on an intermittent fasting regimen, careful consideration and preparation are paramount. It’s not suitable for everyone, and certain individuals should avoid it altogether – including those with a history of eating disorders, pregnant or breastfeeding women, people with type 1 diabetes, and those taking certain medications. A gradual approach is generally recommended to minimize side effects and maximize adherence. Here’s a suggested framework:
- Start slowly: Begin with a less restrictive protocol like the 12/12 method (fasting for 12 hours and eating within a 12-hour window) before gradually increasing the fasting period if tolerated.
- Hydrate adequately: Drinking plenty of water is crucial during both fasting and feeding windows. Dehydration can negate some of the benefits and lead to adverse effects.
- Focus on nutrient density: When you are eating, prioritize whole, unprocessed foods rich in vitamins, minerals, and antioxidants. This provides your body with the nutrients it needs to thrive during periods of restricted eating.
It’s also important to monitor how your body responds and adjust the protocol accordingly. Some common initial side effects include hunger pangs, fatigue, and headaches – these usually subside as the body adapts. Listen to your body’s signals and don’t push yourself beyond your limits. A well-planned 7-Day Meal Plan to Manage Bloating and Improve Digestion can help you navigate these changes successfully.
Combining IF with Other Circulation-Boosting Strategies
Intermittent fasting shouldn’t be viewed in isolation; it works best when integrated into a holistic lifestyle that supports cardiovascular health. Regular exercise remains one of the most powerful tools for improving blood flow, strengthening the heart muscle, and reducing risk factors for cardiovascular disease. Aim for at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic exercise per week, along with strength training exercises twice a week.
Alongside exercise, dietary choices play a vital role. A diet rich in fruits, vegetables, whole grains, lean protein, and healthy fats (like omega-3 fatty acids found in fish) provides the building blocks for healthy blood vessels and supports optimal circulation. Reducing intake of processed foods, sugary drinks, and excessive saturated and trans fats is also essential. Finally, stress management techniques like meditation, yoga, or deep breathing exercises can help lower cortisol levels, which contribute to inflammation and endothelial dysfunction. Incorporating How To Use Herbs And Spices To Support Blood Pressure Control into your diet can further enhance these efforts.
Potential Limitations & Future Research
While the evidence for intermittent fasting’s circulatory benefits is promising, it’s important to acknowledge its limitations. Much of the research has been conducted on animals or in small human studies, and larger, long-term clinical trials are needed to confirm these findings and fully understand the mechanisms involved. The optimal IF protocol – including the ideal fasting duration and frequency – also remains a topic of ongoing investigation.
Furthermore, individual responses to intermittent fasting can vary significantly depending on factors such as genetics, age, activity level, and overall health status. It’s crucial to approach IF with a personalized perspective and seek guidance from a healthcare professional to determine if it’s appropriate for you and how to implement it safely and effectively. Future research should also explore the potential synergistic effects of combining intermittent fasting with other lifestyle interventions like exercise and dietary modifications to maximize its impact on cardiovascular health and overall well-being. The field is evolving rapidly, and we can expect a more comprehensive understanding of IF’s role in promoting healthy circulation as more studies are conducted. Paying attention to Hydration And Blood Pressure: What You Need To Know is also vital for optimal health.