Our bodies are remarkable self-sustaining systems, constantly working to maintain balance – homeostasis. This delicate equilibrium relies on intricate cellular processes, including growth, repair, and removal of damaged components. However, as we age, or when faced with stressors like poor diet, lack of sleep, or environmental toxins, these processes can become less efficient, leading to cellular dysfunction and potentially chronic disease. Increasingly, scientists are discovering that deliberately inducing periods of nutrient scarcity – through practices like intermittent fasting – can powerfully activate the body’s natural cleanup crew, triggering a fundamental process called autophagy, which is essential for both cell health and longevity. This isn’t about deprivation; it’s about strategically leveraging the body’s inherent mechanisms to optimize cellular function.
Autophagy, literally meaning “self-eating,” might sound alarming, but it’s a critical part of life. It’s the way our cells recycle damaged components – misfolded proteins, dysfunctional organelles – essentially dismantling and reusing them for energy or building new structures. Think of it as an internal quality control system, preventing buildup of cellular debris that can contribute to aging and disease. When we constantly feed our bodies, particularly with nutrient-rich foods, autophagy is less frequently activated. The cell remains in a growth/building mode. However, when nutrients become scarce, the cell switches gears, initiating autophagy as a survival mechanism. This process isn’t limited to times of famine; it’s happening continuously at low levels but can be significantly enhanced through targeted strategies like fasting impacts.
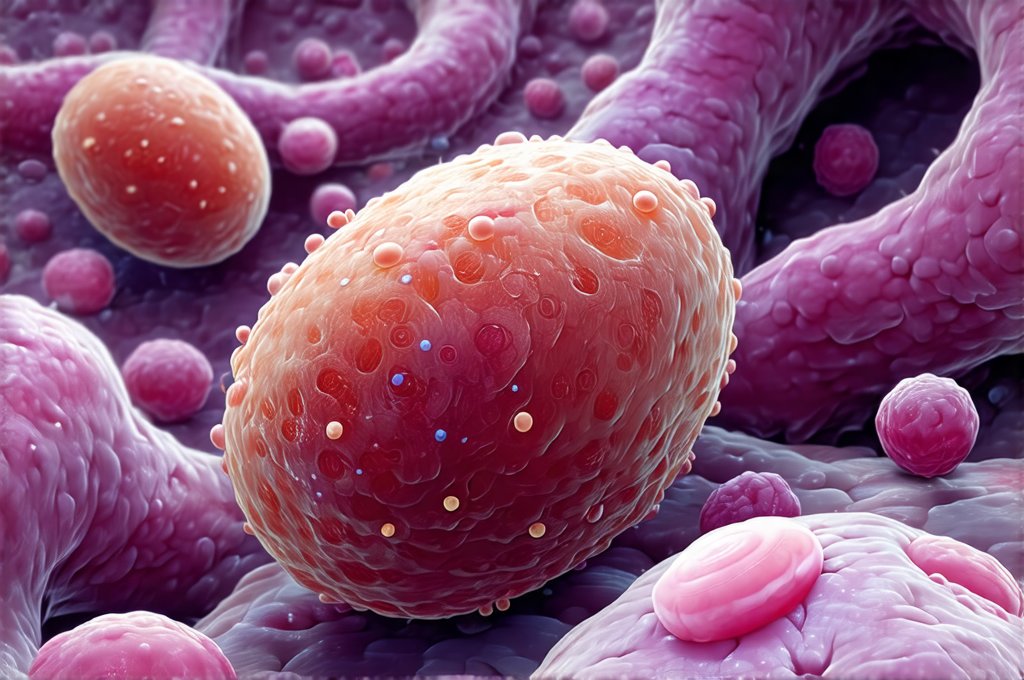
Autophagy: The Cellular Recycling System
Autophagy isn’t one single event, but rather a complex multi-step process with different forms. There are three main types: macroautophagy (the most studied), microautophagy and chaperone-mediated autophagy. Macroautophagy is what’s typically referred to when discussing fasting and cellular health. This involves the formation of a double-membraned vesicle called an autophagosome which engulfs damaged or unnecessary cellular components. These autophagosomes then fuse with lysosomes, acting as the cell’s “recycling centers,” where the contents are broken down into their basic building blocks for reuse.
The beauty of autophagy lies in its efficiency and adaptability. It’s not just about clearing out debris; it also plays a vital role in immune function by eliminating intracellular pathogens (bacteria, viruses). Furthermore, it’s crucial for development – shaping cells during embryogenesis – and maintaining tissue homeostasis. The process is tightly regulated by various signaling pathways within the cell, responding to changes in nutrient availability, stress levels, and hormonal signals. Disruptions in autophagy have been linked to a wide range of diseases including neurodegenerative disorders (Alzheimer’s, Parkinson’s), cancer, and autoimmune conditions.
Fasting acts as one of the most potent stimuli for activating macroautophagy. When food intake is reduced or eliminated, cellular energy demands shift. The body begins tapping into stored reserves and simultaneously initiates autophagy to provide building blocks and energy from recycled components. This process isn’t immediate; it typically takes several hours – often 12-24 hours – of fasting before significant autophagic activity can be observed. The duration and type of fast (intermittent, prolonged) can influence the extent of autophagy induced. It’s important to note that while fasting is a powerful tool, it’s not a one-size-fits-all approach and should be approached cautiously based on individual health status.
Cellular Repair Mechanisms Activated by Fasting
Beyond autophagy, fasting triggers several other cellular repair mechanisms designed to maintain optimal function. One key process is mitophagy, specifically the selective removal of damaged mitochondria – the powerhouses of our cells. Dysfunctional mitochondria generate harmful reactive oxygen species (ROS) and contribute to cellular aging. By selectively clearing out these defective mitochondria, mitophagy improves energy production and reduces oxidative stress. Fasting stimulates both autophagy generally and mitophagy specifically, offering a dual benefit for mitochondrial health.
Another important pathway activated during fasting is DNA repair. When cells are under stress – including nutrient scarcity – they prioritize repairing damaged DNA to ensure genomic stability. This involves activating various enzymes involved in identifying and correcting errors in the DNA code. The reduced metabolic rate associated with fasting also minimizes oxidative damage, further supporting efficient DNA repair processes. Essentially, fasting gives the cell a chance to focus its resources on maintenance and repair rather than constant digestion and growth.
Finally, fasting can promote cellular resilience through hormesis. Hormesis refers to the idea that mild stress – like that induced by intermittent fasting – can actually strengthen cells, making them more resistant to future stressors. This is similar to how exercise strengthens muscles; it involves a controlled disruption of homeostasis followed by adaptation and improved function. The body responds to the temporary challenge of fasting by upregulating antioxidant defenses, improving protein quality control, and enhancing overall cellular robustness.
Intermittent Fasting Protocols & Autophagy
Intermittent fasting (IF) isn’t about starving yourself. It’s a pattern of eating that cycles between periods of voluntary fasting and non-fasting on a regular schedule. There are several common IF protocols:
- Time-Restricted Eating: This involves limiting your eating window to a specific number of hours each day, such as 16/8 (16 hours fasting, 8 hours eating) or 18/6.
- 5:2 Diet: Eating normally for five days a week and restricting calorie intake to around 500-600 calories on two non-consecutive days.
- Alternate-Day Fasting: Alternating between days of normal eating and days of severely restricted calorie intake or complete fasting.
The optimal IF protocol varies depending on individual goals, lifestyle, and health status. For maximizing autophagy, longer fasting periods seem to be more effective – potentially 16-24 hours or even longer for experienced fasters under appropriate guidance. However, shorter intermittent fasts (12-16 hours) can still offer significant benefits. It’s crucial to listen to your body and avoid pushing yourself beyond comfortable limits. Gradual implementation is key; starting with a shorter fasting window and gradually increasing it over time allows the body to adapt more easily.
It’s also important to understand that what you eat during your eating windows matters. Focusing on nutrient-dense foods – whole, unprocessed foods rich in vitamins, minerals, and antioxidants – supports cellular repair and maximizes the benefits of IF. Avoid excessive sugar, processed foods, and unhealthy fats, which can counteract the positive effects of fasting. Staying hydrated is also essential, as water plays a vital role in all cellular processes including autophagy.
Considerations & Cautions Regarding Fasting
While research suggests that fasting can be incredibly beneficial, it’s not appropriate for everyone. Individuals with certain medical conditions – such as diabetes, eating disorders, or adrenal fatigue – should consult with a healthcare professional before attempting any form of intermittent fasting. Pregnant or breastfeeding women and individuals taking medication also need to exercise caution and seek medical guidance.
Fasting can have side effects, particularly during the initial adaptation phase. These may include headaches, fatigue, irritability, and digestive issues. These symptoms are usually temporary and can be minimized by staying hydrated, gradually increasing fasting periods, and ensuring adequate nutrient intake during eating windows. It’s also crucial to prioritize sleep and manage stress levels, as both factors significantly impact cellular health and the body’s ability to adapt to fasting.
Ultimately, fasting is a tool – not a cure-all. It should be integrated into a holistic lifestyle that includes a balanced diet, regular exercise, adequate sleep, and effective stress management techniques. Viewing it as part of a comprehensive approach to health and well-being is far more likely to yield sustainable positive results than viewing it as a quick fix or restrictive diet. Consider pairing proteins with carbs for digestive ease during eating windows. The goal isn’t simply to fast; it’s to optimize cellular function and promote long-term health through strategic nutrient timing and activation of the body’s natural repair mechanisms. And if you find yourself struggling, remember how to stop snacking while still feeling satisfied! Finally, for those navigating dietary restrictions, exploring rice, oats, and potatoes within an IBS diet can be helpful.