Fasting has surged in popularity as both a wellness trend and a dietary approach, attracting individuals seeking potential benefits ranging from weight management to improved metabolic health. Simultaneously, hormonal birth control remains a widespread method of contraception and is often prescribed for conditions beyond pregnancy prevention, such as managing menstrual irregularities or reducing endometriosis symptoms. This intersection raises a crucial question: can you safely fast while taking birth control pills? The answer isn’t straightforward, as it depends on the type of fasting, the specific birth control pill formulation, individual health factors, and potential interactions between the two. Navigating this requires careful consideration and ideally, consultation with a healthcare professional to ensure safety and avoid unintended consequences.
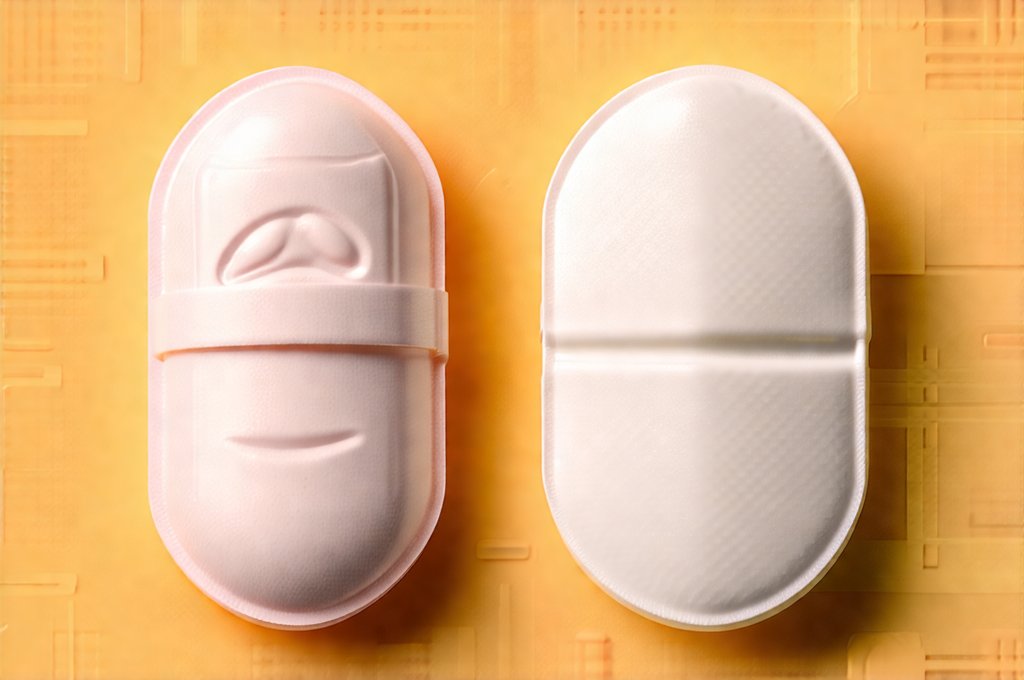
The complexity stems from how fasting impacts the body – specifically, nutrient absorption, hormonal balance, and metabolic processes – and how these changes might interact with the hormones delivered by birth control pills. Birth control pills already influence hormone levels, and introducing periods of restricted eating can further disrupt this delicate equilibrium. Furthermore, different types of birth control (pills containing estrogen and progestin versus progestin-only pills) behave differently within the body, making a one-size-fits-all answer impossible. Understanding these nuances is key to making informed decisions about incorporating fasting into your lifestyle while on hormonal contraception.
Types of Fasting and Their Potential Impact
Fasting isn’t simply not eating; it encompasses a spectrum of approaches with varying degrees of restriction and duration. Intermittent fasting (IF), arguably the most popular form, involves cycling between periods of voluntary fasting and non-fasting on a regular schedule. Common IF methods include: 16/8 (fasting for 16 hours, eating within an 8-hour window), 5:2 (eating normally five days a week and restricting calories to around 500-600 two days a week) and alternate-day fasting. More extended fasts, lasting 24 hours or longer, are less common and generally require medical supervision. Each method places different physiological demands on the body.
The primary concern with fasting while on birth control is potential interference with pill absorption. Estrogen and progestin are often absorbed in the small intestine, and factors that affect gastrointestinal motility or nutrient uptake can reduce their effectiveness. While studies specifically examining this interaction are limited, prolonged periods without food could theoretically decrease absorption, particularly if the pill is taken during a fasting window. This is less of a concern with consistently timed IF schedules where pills are always taken during an eating window but needs to be considered. Furthermore, significant calorie restriction can impact liver function, which plays a role in metabolizing hormones; this is more pertinent for longer fasts or very restrictive diets. It may be helpful to review low-sodium sauces and dressings when planning meals during eating windows.
It’s important to remember that birth control pills themselves can affect appetite and metabolism. Some individuals experience changes in hunger levels when starting hormonal contraception, making it potentially harder to adhere to fasting schedules. Conversely, the metabolic alterations induced by fasting might influence how the body processes hormones from the pill, although the exact nature of this interaction remains largely unexplored. Ultimately, consistent monitoring and open communication with a healthcare provider are crucial for assessing individual responses.
Considerations for Progestin-Only Pills (“Mini-Pills”)
Progestin-only pills (POPs), often referred to as “mini-pills,” have a narrower window of opportunity for effective absorption compared to combination pills. They must be taken at approximately the same time each day, ideally within a 3-hour timeframe, to maintain consistent hormone levels and prevent pregnancy. This timing is critical because POPs rely on thickening cervical mucus to prevent sperm from reaching the egg – this effect diminishes if the pill isn’t taken consistently.
Fasting can introduce complexities for mini-pill users due to the increased risk of absorption interference. Even relatively short fasting periods, especially if they disrupt meal times or are combined with gastrointestinal issues (like diarrhea), could potentially reduce efficacy. The impact is amplified by factors such as delayed gastric emptying or changes in intestinal motility caused by fasting. Therefore, individuals on mini-pills should be particularly cautious about incorporating intermittent fasting and prioritize consistent pill timing over rigid adherence to a fasting schedule.
Maintaining strict adherence to the 3-hour window is paramount. If you choose to fast, consider taking your mini-pill with a small snack or meal during your eating window to maximize absorption. It’s vital to have a backup contraception plan available in case of concerns about pill efficacy and consult your healthcare provider to discuss potential adjustments to your fasting regimen or contraceptive method. Individuals transitioning off birth control may also find the PCOS reset plan helpful in managing hormonal shifts.
Impact on Nutrient Absorption & Electrolyte Balance
Fasting, by its nature, restricts food intake, potentially leading to deficiencies in essential vitamins and minerals. While well-planned intermittent fasting protocols often aim to minimize nutrient loss, prolonged fasts or highly restrictive diets can exacerbate these concerns. Birth control pills can also subtly affect nutrient levels; for instance, some formulations may increase the need for certain B vitamins. Combining both introduces a risk of compounding nutritional deficiencies.
The body requires adequate intake of electrolytes – sodium, potassium, and magnesium – to function properly. Fasting can disrupt electrolyte balance due to reduced dietary intake and alterations in kidney function. This imbalance can lead to symptoms like fatigue, muscle cramps, dizziness, and even more severe health issues. Birth control pills themselves have been linked to subtle changes in electrolyte metabolism in some individuals, potentially increasing the risk of imbalances during fasting.
To mitigate these risks, if you choose to fast while on birth control, focus on nutrient-dense foods during your eating windows. Consider supplementing with a multivitamin or specific nutrients as recommended by your healthcare provider. Staying adequately hydrated and paying attention to electrolyte intake (through food or supplementation) are also essential steps to maintain overall health. For those dealing with digestive sensitivities, exploring IBS-friendly recipes can support gut health during fasting periods.
Monitoring for Side Effects & Communication with Your Doctor
The most crucial aspect of fasting while on birth control is diligent self-monitoring and open communication with your doctor. Pay close attention to any changes in your body, both physical and emotional. Common side effects to watch out for include: irregular bleeding, spotting between periods, changes in mood or energy levels, increased anxiety, digestive issues (bloating, constipation), and disruptions in sleep patterns. These symptoms could indicate that fasting is interfering with hormone levels or pill efficacy.
If you experience any concerning side effects, immediately stop the fast and contact your healthcare provider. Do not attempt to self-diagnose or adjust your medication without professional guidance. Be prepared to discuss your fasting schedule, birth control type, and any other relevant health information during your consultation. Your doctor can assess whether fasting is appropriate for you, recommend adjustments to your regimen, or explore alternative contraceptive options if necessary.
Boldly stated, prioritizing safety and well-being should always be the primary concern when combining hormonal contraception with dietary changes like fasting. A proactive approach involving regular check-ins with a healthcare professional is paramount in ensuring that both your health and reproductive goals are protected. If you’re unsure about what to eat during eating windows, quick bloat-reducing meals may provide some inspiration.