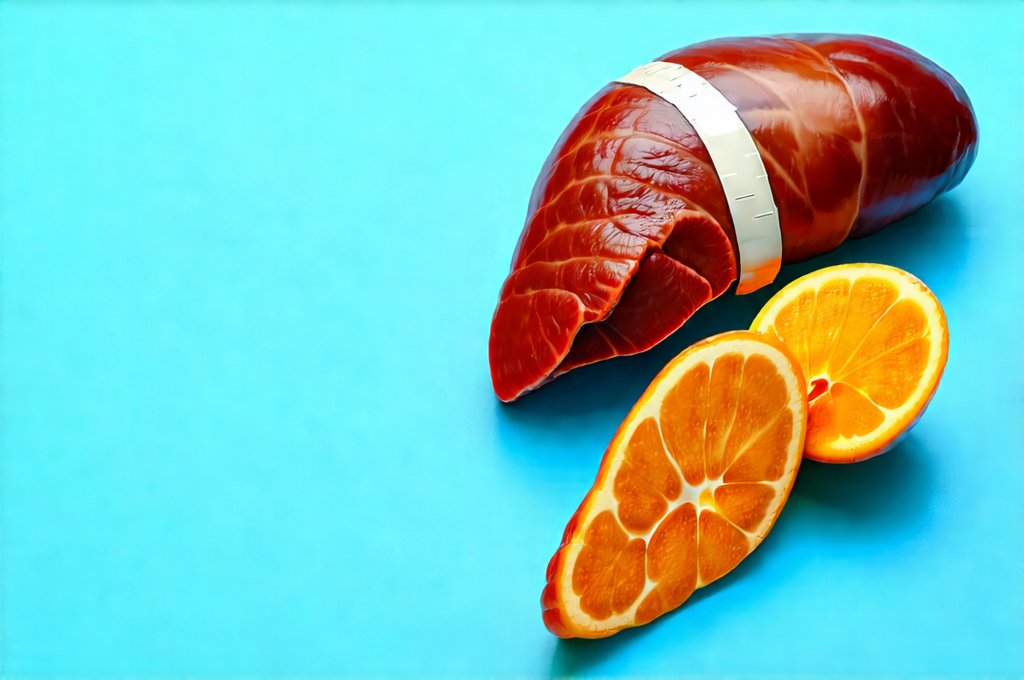
The liver is arguably the body’s most versatile chemical processing plant, constantly working to filter blood, metabolize nutrients, synthesize proteins, and eliminate waste products. It’s an organ under constant strain in modern life, bombarded by environmental toxins, processed foods, and metabolic byproducts. Consequently, supporting optimal liver function is crucial for overall health and wellbeing. Many strategies are promoted as “liver detoxes,” ranging from juice cleanses to specialized diets. However, a more nuanced approach focuses on supporting the liver’s natural detoxification pathways rather than attempting drastic or unscientific interventions. This means providing it with the resources it needs – adequate nutrition, hydration, and reduced stressors – to function at its best.
Intermittent fasting (IF) has gained significant popularity as a dietary strategy for weight management and metabolic health. But beyond these well-publicized benefits, emerging research suggests that IF may also positively influence liver detoxification processes. This isn’t about “detoxing” in the popular sense; it’s about creating physiological conditions – periods of reduced digestive workload and cellular repair – that allow the liver to operate more efficiently. The concept revolves around strategically cycling between periods of eating and voluntary fasting, which can have profound effects on metabolic regulation and cellular health. Understanding how IF interacts with the liver’s intrinsic detoxification systems is key to appreciating its potential benefits for long-term wellbeing. For example, understanding if can intermittent fasting worsen acid reflux is important before starting.
Intermittent Fasting & Liver Metabolism
Intermittent fasting isn’t a new concept; humans evolved in environments where food availability wasn’t constant. Our bodies are, therefore, equipped to handle periods of fasting. The metabolic shift that occurs during IF is particularly relevant to liver health. When we eat frequently throughout the day, the liver is constantly engaged in processing incoming nutrients. This can place a sustained burden on its detoxification pathways. Conversely, during fasting, digestive processes slow down dramatically, giving the liver a chance to focus on other crucial functions – including clearing out accumulated toxins and repairing cellular damage. This isn’t about starving the body; it’s about providing strategic breaks for optimal function.
The core principle behind IF’s metabolic benefits lies in its impact on insulin sensitivity. Chronically elevated insulin levels, often caused by frequent carbohydrate intake, can contribute to insulin resistance, a precursor to many chronic diseases. Insulin resistance also impacts liver health, promoting fat accumulation within the liver (non-alcoholic fatty liver disease or NAFLD). IF helps improve insulin sensitivity by reducing overall glucose exposure and forcing the body to utilize stored energy sources – primarily fats – for fuel. This reduction in insulin levels allows the liver to shift its focus from glucose metabolism to detoxification and repair processes.
Furthermore, IF promotes autophagy, a cellular “self-cleaning” process where damaged or dysfunctional cells are broken down and recycled. Autophagy is crucial for maintaining cellular health and preventing the accumulation of toxic proteins within the liver. Fasting triggers autophagy by reducing nutrient signaling, essentially telling the body to conserve energy and eliminate unnecessary components. This cleanup process can significantly enhance liver function and protect against long-term damage. You may also want to explore a targeted pcos plan to further support your liver health.
The Role of AMPK Activation
A key molecular player in mediating many of IF’s beneficial effects is AMPK (adenosine monophosphate-activated protein kinase). AMPK acts as a cellular energy sensor, becoming activated when energy levels are low – precisely what happens during fasting. When activated, AMPK promotes glucose uptake in muscle cells, enhances fat burning, and inhibits hepatic gluconeogenesis (the production of glucose by the liver). This multifaceted action contributes to improved insulin sensitivity and metabolic health.
- AMPK activation also directly supports liver detoxification pathways.
- It increases the expression of genes involved in glutathione synthesis – a master antioxidant essential for neutralizing toxins.
- AMPK stimulates mitochondrial biogenesis, leading to healthier and more efficient mitochondria within liver cells. Mitochondria are vital for energy production and detoxification processes.
The connection between IF, AMPK activation, and enhanced liver function is increasingly recognized as a critical mechanism underlying its health benefits. It’s not simply about restricting calories; it’s about triggering specific cellular responses that promote metabolic flexibility and resilience. Those looking to lose fat may also find can intermittent fasting help you lose fat beneficial, alongside liver support.
Gut Microbiome & Liver Detoxification
The gut microbiome – the trillions of bacteria residing in our digestive tract – plays an unexpectedly significant role in liver detoxification. A healthy, diverse gut microbiome helps modulate inflammation, improve nutrient absorption, and reduce the burden on the liver. Conversely, a dysbiotic gut (an imbalance in bacterial populations) can lead to increased intestinal permeability (“leaky gut”), allowing toxins to enter the bloodstream and overwhelm the liver.
Intermittent fasting can positively influence the gut microbiome by altering the composition of bacteria. During periods of fasting, harmful bacteria tend to decline while beneficial bacteria – those that produce short-chain fatty acids (SCFAs) like butyrate – may flourish. SCFAs are vital for gut health and have anti-inflammatory properties, reducing the inflammatory load on the liver.
Moreover, IF can help reduce inflammation in the gut, further improving intestinal barrier function. A stronger gut barrier means fewer toxins reaching the liver, allowing it to focus on its core detoxification functions more effectively. The interplay between IF, gut microbiome health, and liver detoxification highlights the interconnectedness of these systems. Improving gut health can significantly improve overall wellbeing.
Considerations & Practical Implementation
While IF shows promise for supporting liver detoxification pathways, it’s not a one-size-fits-all solution. Several factors need to be considered before adopting an IF protocol:
- Individual Health Status: Individuals with certain medical conditions – such as diabetes, eating disorders, or adrenal fatigue – should consult with a healthcare professional before starting IF.
- Medication Interactions: Fasting can affect how medications are absorbed and metabolized. It’s crucial to discuss potential interactions with your doctor.
- Gradual Introduction: Don’t jump into a strict IF schedule immediately. Start with a shorter fasting window (e.g., 12-hour fast) and gradually increase it as tolerated.
Common IF protocols include:
1. 16/8 Method: Fasting for 16 hours and confining eating to an 8-hour window.
2. 5:2 Diet: Eating normally five days a week and restricting calories (around 500-600 calories) on two non-consecutive days.
3. Alternate-Day Fasting: Alternating between days of normal eating and days of very low calorie intake or complete fasting.
Hydration is paramount during IF, as it helps flush out toxins and supports kidney function. Focusing on a whole-food diet rich in fruits, vegetables, lean protein, and healthy fats provides the liver with essential nutrients for optimal detoxification. It’s also important to minimize exposure to environmental toxins – such as pesticides, heavy metals, and processed foods – to reduce the liver’s workload. Ultimately, IF is best viewed as one component of a holistic lifestyle approach to supporting liver health. A nutrition plan can also be useful for those seeking more structured support.