The digestive system is often taken for granted until something goes wrong. For many individuals struggling with conditions like IBS, bloating, constipation, or simply chronic discomfort, daily life can be significantly impacted by gut health. It’s easy to fall into patterns that exacerbate these issues – quick meals, processed foods, stress eating – but a proactive and thoughtfully designed eating strategy can often make a remarkable difference. This isn’t about restrictive diets or eliminating entire food groups; it’s about understanding how different dietary choices influence the complex ecosystem within your gut and learning to nourish it effectively for consistent relief and improved wellbeing.
A truly effective daily eating strategy focuses on building long-term, sustainable habits rather than quick fixes. It requires a degree of self-awareness – paying attention to how your body responds to various foods – and adapting principles to fit individual needs and tolerances. The goal isn’t perfection; it’s progress towards a more comfortable and balanced digestive experience. This article will explore practical approaches, focusing on core concepts and actionable steps you can integrate into your daily routine to promote consistent gut relief, understanding that everyone’s journey is unique and requires personalized adjustments.
Foundational Dietary Principles for Gut Health
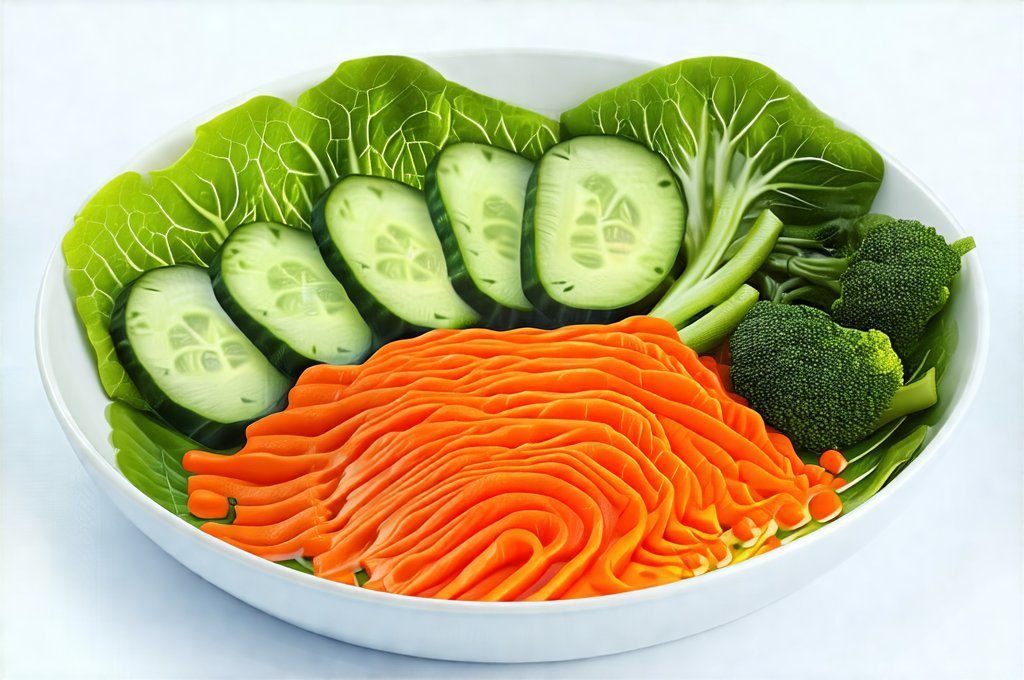
A healthy gut thrives on diversity – not just of the bacteria within it, but also of the nutrients it receives. Many common digestive issues stem from a lack of fiber, inadequate hydration, and an overabundance of processed foods. Therefore, the cornerstone of any gut-relief eating strategy must be centered around whole, unprocessed foods. This means prioritizing fruits, vegetables, lean proteins, healthy fats, and complex carbohydrates while minimizing refined sugars, excessive saturated and trans fats, and artificial additives. Focusing on food quality is often more impactful than focusing solely on quantity.
The importance of fiber cannot be overstated. It acts as a prebiotic – essentially feeding the beneficial bacteria in your gut – and helps regulate bowel movements. Aim for a variety of fiber sources, including soluble fiber (found in oats, beans, apples) which absorbs water and softens stool, and insoluble fiber (found in whole grains, vegetables) which adds bulk and promotes regularity. However, increasing fiber intake too quickly can actually worsen symptoms; it’s crucial to gradually increase your intake while staying adequately hydrated.
Hydration is equally vital. Water helps move food through the digestive tract, preventing constipation and supporting optimal gut function. Aim for at least eight glasses of water per day, although individual needs may vary based on activity level and climate. Consider incorporating herbal teas or infused water as enjoyable ways to increase your fluid intake. Beyond water, mindful eating practices are essential. This means slowing down during meals, chewing thoroughly, and paying attention to hunger and fullness cues. Rushing through meals can lead to incomplete digestion and increased discomfort.
Identifying Trigger Foods & Food Intolerances
One of the most impactful steps towards gut relief is identifying foods that trigger your symptoms. These aren’t necessarily allergies; they could be intolerances or sensitivities that cause inflammation or disruption in your digestive process. Common culprits include dairy, gluten, fructose (found in many fruits and sweeteners), lactose, certain FODMAPs (Fermentable Oligosaccharides, Disaccharides, Monosaccharides And Polyols – more on those later), and artificial sweeteners.
A helpful approach is to keep a detailed food diary for a week or two, recording everything you eat and drink, along with any associated symptoms (bloating, gas, diarrhea, constipation, abdominal pain). Look for patterns between specific foods and your digestive distress. You can then try an elimination diet – removing suspected trigger foods from your diet for a period of time (typically 2-4 weeks) and gradually reintroducing them one by one to see if symptoms return. This process should ideally be guided by a healthcare professional, but it can provide valuable insights into your individual sensitivities.
It’s important to remember that food intolerances can change over time. A food that bothered you six months ago might not cause issues now, and vice versa. Regular self-assessment and adjustments to your diet are key. Don’t assume a blanket approach works for everyone; your gut is unique, and its needs will evolve. Understanding daily eating habits can greatly improve digestion.
The Role of FODMAPs
FODMAPs are short-chain carbohydrates that can be poorly absorbed in the small intestine, leading to fermentation by bacteria in the large intestine and potentially causing gas, bloating, and discomfort. While not inherently bad for everyone, individuals with IBS or sensitive digestive systems often benefit from a low-fodmap diet – at least temporarily.
This isn’t about eliminating FODMAPs forever; it’s more about identifying which ones specifically trigger your symptoms. Common high-FODMAP foods include:
* Onions and garlic
* Apples, pears, mangoes
* Wheat and rye products
* Dairy products (containing lactose)
* Legumes (beans, lentils)
A low-FODMAP diet typically involves a strict elimination phase followed by a carefully controlled reintroduction phase. Again, it’s best to work with a registered dietitian or healthcare provider when implementing a low-FODMAP diet to ensure you’re still getting adequate nutrients and avoiding unnecessary restrictions. The goal is to identify your specific FODMAP triggers, not eliminate all of them permanently.
Probiotics & Prebiotics: Nourishing Your Gut Microbiome
Probiotics are live microorganisms that can benefit gut health when consumed in sufficient quantities. They’re found in fermented foods like yogurt (with live and active cultures), kefir, sauerkraut, kimchi, and kombucha. Supplementing with probiotics can also be helpful, but it’s important to choose a high-quality product with strains specifically suited to your needs.
Prebiotics, as mentioned earlier, are the food source for these beneficial bacteria. They’re found in fiber-rich foods like onions, garlic, leeks, asparagus, bananas, and oats. Combining probiotics and prebiotics – often referred to as synbiotics – can create a synergistic effect, promoting a more diverse and thriving gut microbiome.
However, simply taking probiotics isn’t a magic bullet. The effectiveness of probiotics depends on many factors, including the specific strains used, the dosage, and your individual gut composition. It’s best to focus on incorporating fermented foods into your diet regularly as a natural source of probiotics, alongside a fiber-rich diet that supports their growth and activity. Remember to introduce both gradually to avoid any temporary digestive upset. For more information about improving digestion through food choices, consider reviewing best smoothies. A simple clean day can also be beneficial for gut health and overall wellbeing.
It is important to note that this information is for general knowledge and informational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.