Diabetes management is often seen as restrictive, filled with lists of ‘don’ts’ and limitations. However, adopting a dietary approach doesn’t have to equate to deprivation. In fact, focusing on abundance – specifically, an abundance of whole, unprocessed foods – can be incredibly empowering and beneficial for overall health, including blood sugar control. This is where the Mediterranean Diet comes in, offering not just a meal plan but a lifestyle centered around vibrant flavors, social connection through food, and sustained well-being. It’s about building a relationship with your food that prioritizes nourishment and enjoyment, rather than rigid restriction.
The traditional Mediterranean diet isn’t specifically designed for diabetes management, but its inherent characteristics align beautifully with the nutritional needs of individuals living with this condition. The emphasis on healthy fats, fiber-rich carbohydrates, lean proteins, and limited processed sugars naturally supports stable blood glucose levels, reduces inflammation, and promotes heart health – all crucial aspects of diabetes care. Adapting this time-tested dietary pattern for those managing diabetes requires a thoughtful approach, focusing on portion control and mindful food choices to maximize its benefits while staying within individual needs and preferences. It’s about making informed adjustments, not wholesale changes that feel unsustainable.
Understanding the Core Principles of a Diabetes-Friendly Mediterranean Diet
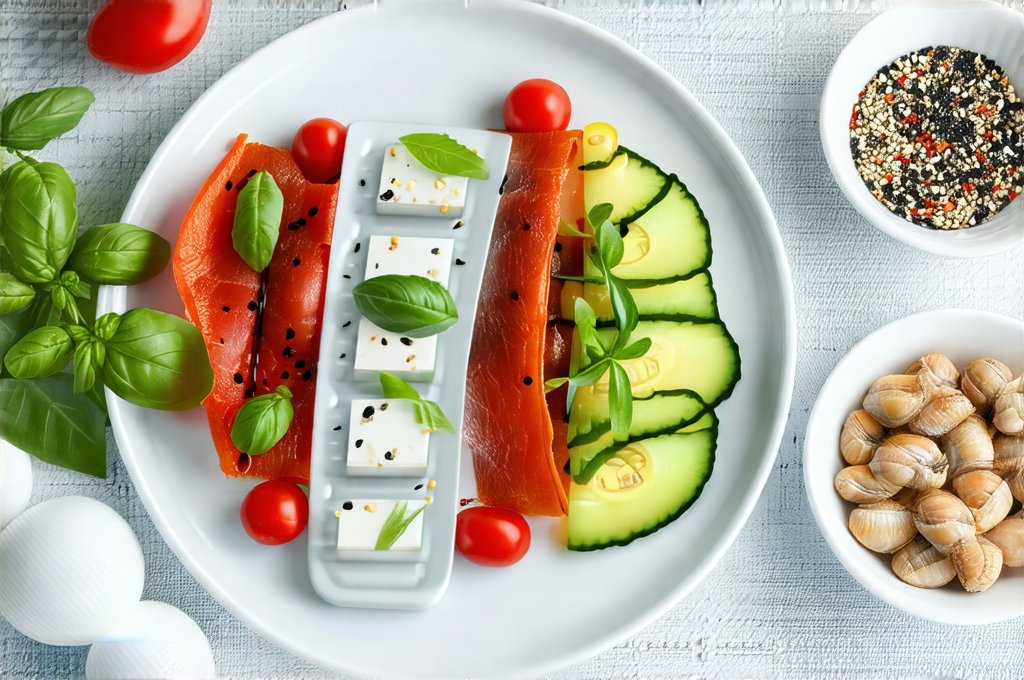
The foundation of this diet lies in prioritizing whole foods over processed alternatives. Think of it as building your meals around what grows – fruits, vegetables, legumes, nuts, seeds, and whole grains. Olive oil is the primary source of fat, offering healthy monounsaturated fats that are beneficial for heart health and can improve insulin sensitivity. Lean proteins like fish, poultry (in moderation), and beans take center stage, while red meat consumption is limited to occasional servings. Dairy products, if included, should be consumed in moderate amounts, preferably opting for low-fat or Greek yogurt options. Hydration is also key; water should be the beverage of choice.
This isn’t about eliminating food groups entirely but rather focusing on quality and quantity. The Mediterranean diet embraces flavor – herbs and spices are used generously instead of excessive salt or sugar. This approach makes it easier to adhere to long-term, as it’s less about deprivation and more about discovering new culinary experiences. A key element is mindful eating: paying attention to hunger cues, savoring each bite, and stopping when satisfied, rather than overfull. This helps regulate portion sizes and promotes a healthier relationship with food.
The beauty of the Mediterranean diet lies in its flexibility. It’s not a rigid set of rules but a framework that can be adapted to individual preferences and cultural backgrounds. For someone managing diabetes, this means tailoring portion sizes based on carbohydrate counting or glycemic index considerations, while still enjoying the core principles of the diet. It’s about finding what works for you and building sustainable habits that support your health goals.
Navigating Carbohydrates in a Mediterranean Context
Carbohydrate management is often central to diabetes care, but the Mediterranean Diet offers a nuanced approach that differs from strict low-carb diets. It doesn’t advocate for eliminating carbohydrates entirely; instead, it emphasizes choosing complex carbohydrates – those found in whole grains, fruits, vegetables, and legumes – over simple sugars and refined grains. These complex carbs are digested more slowly, leading to a gradual rise in blood glucose levels, preventing spikes and crashes.
Fiber plays a crucial role here. Foods rich in fiber slow down digestion, further contributing to stable blood sugar control. Legumes (beans, lentils), whole grains like quinoa and barley, and non-starchy vegetables are excellent sources of fiber. Portion control is still essential, even with healthy carbohydrates. Understanding your individual carbohydrate tolerance and working with a registered dietitian or certified diabetes educator can help determine appropriate serving sizes.
It’s also important to consider the glycemic index (GI) and glycemic load (GL) of foods. While GI measures how quickly a food raises blood sugar, GL takes into account both the GI and the amount of carbohydrate in a typical serving. Choosing foods with lower GI and GL values can help manage blood glucose levels more effectively. However, focusing solely on these numbers isn’t enough; the overall nutritional quality of the food is equally important.
Meal Planning for Blood Sugar Stability
Planning your meals ahead of time is one of the most effective strategies for managing diabetes, and the Mediterranean diet lends itself well to this approach. Here’s a step-by-step guide:
- Start with Protein: Begin by choosing a lean protein source like grilled fish, chicken breast, or lentil stew.
- Add Non-Starchy Vegetables: Fill half your plate with colorful non-starchy vegetables such as broccoli, spinach, peppers, or zucchini.
- Include Complex Carbohydrates: Add a moderate portion of complex carbohydrates like quinoa, brown rice, or sweet potato (consider portion size based on individual needs).
- Finish with Healthy Fats: Drizzle with olive oil and sprinkle with nuts or seeds for healthy fats.
This method ensures balanced meals that provide sustained energy and minimize blood sugar spikes. Utilizing meal prepping techniques – preparing ingredients in advance or cooking larger batches of food – can save time and make it easier to stick to your plan throughout the week. Don’t be afraid to experiment with different recipes and flavors within these guidelines to keep things interesting and enjoyable.
Snacking Smartly
Snacks are often necessary for maintaining stable blood sugar levels, especially between meals. The key is to choose snacks that combine protein, fiber, and healthy fats. Avoid sugary drinks, processed snack foods, and large portions of refined carbohydrates. Here are some diabetes-friendly Mediterranean snack options:
- A small handful of almonds or walnuts with a piece of fruit
- Greek yogurt with berries and a sprinkle of chia seeds
- Vegetable sticks (carrots, celery) with hummus
- Whole-grain crackers with avocado and a slice of tomato
- Hard-boiled egg with a side of cucumber slices
Planning your snacks in advance can prevent impulsive choices and ensure you’re fueling your body with nutritious options. Remember to consider the carbohydrate content of your snack and adjust portion sizes accordingly.
Staying Hydrated & Mindful Eating Practices
Water is essential for overall health, including blood sugar control. Aim to drink at least eight glasses of water per day, especially before, during, and after meals. Staying hydrated helps regulate digestion and can prevent dehydration which can sometimes mimic hunger cues. Beyond hydration, cultivating mindful eating habits is crucial.
- Eat slowly and savor each bite
- Pay attention to your body’s hunger and fullness signals
- Minimize distractions during meal times (TV, phone)
- Avoid emotional eating – address underlying emotions rather than turning to food for comfort
- Practice gratitude for the nourishment that food provides
These practices promote a healthier relationship with food and can help you make more informed choices. Remember, diabetes management is about creating sustainable lifestyle changes, not quick fixes. By embracing the principles of the Mediterranean diet and incorporating mindful eating habits, you can take control of your health and enjoy a fulfilling life.