The gut lining is often overlooked, yet it’s arguably one of the most critical components of our overall health. This intricate barrier acts as a gatekeeper, meticulously controlling what enters our bloodstream – nutrients we need to thrive and potential toxins that could trigger inflammation and illness. When this barrier becomes compromised, commonly referred to as “leaky gut,” it can lead to a cascade of issues ranging from digestive distress and autoimmune responses to chronic fatigue and mood imbalances. Many factors can contribute to a weakened gut lining, including stress, poor diet, antibiotic use, and – for some individuals – gluten consumption. Addressing these underlying causes is key to restoring gut health, and for those sensitive to gluten, adopting a well-planned gluten-free approach can be a powerful step towards healing.
This article will explore the connection between gluten, gut health, and the potential benefits of a gluten-free plan focused on rebuilding a healthy gut lining. It’s important to note that gluten sensitivity isn’t always about celiac disease; many people experience non-celiac gluten sensitivity (NCGS), where gluten triggers symptoms without causing the same autoimmune response as celiac. Identifying individual sensitivities and tailoring dietary changes accordingly is paramount, but for those who suspect gluten may be contributing to gut issues, understanding how a thoughtfully implemented gluten-free plan can support healing is invaluable. We’ll cover practical steps, food choices, and strategies beyond simply eliminating gluten to truly nurture your gut lining back to health.
Understanding the Gut Lining & Gluten’s Impact
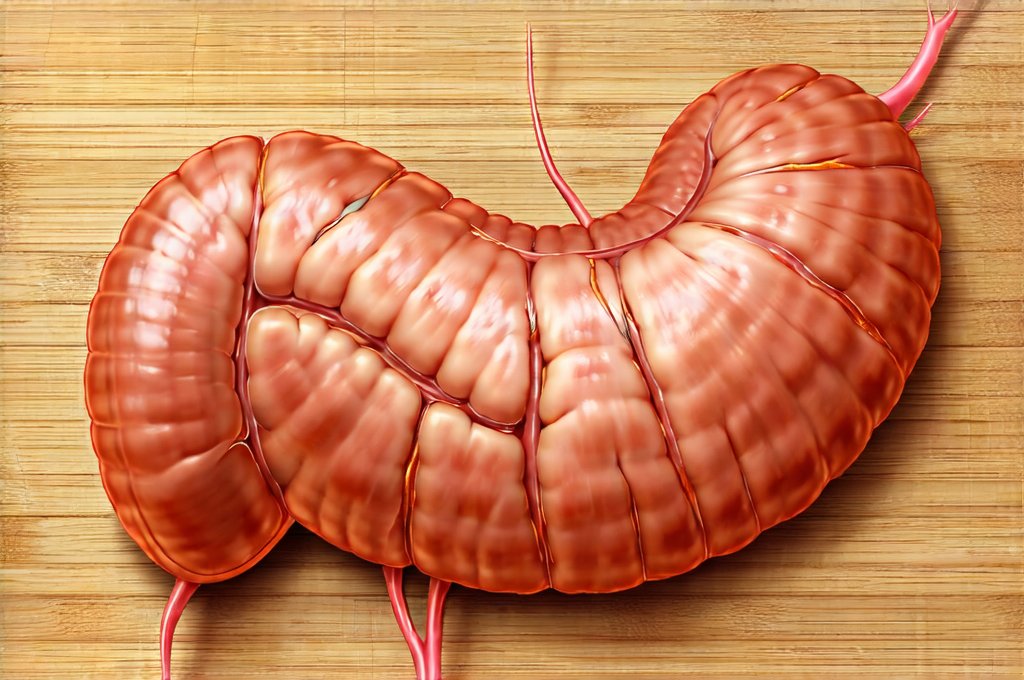
The gut lining isn’t just one layer; it’s a complex ecosystem comprised of tightly joined cells, mucus production, beneficial bacteria (the microbiome), and immune cells. These elements work together to maintain intestinal permeability – the ability to allow nutrients through while blocking harmful substances. When this system is functioning optimally, it provides robust protection against inflammation and supports overall health. However, certain factors can disrupt this delicate balance. Gluten, a protein found in wheat, barley, and rye, has been implicated as one such factor for susceptible individuals.
For those with celiac disease, gluten triggers an autoimmune response that directly attacks the small intestine, damaging the villi (tiny finger-like projections) responsible for nutrient absorption. Even without celiac disease, gluten can contribute to increased intestinal permeability in sensitive individuals through several mechanisms. It may trigger inflammation, disrupt the microbiome, and interfere with digestive enzymes. This disruption allows larger molecules – undigested food particles, toxins, bacteria – to cross the gut barrier and enter the bloodstream, triggering an immune response and potentially leading to systemic inflammation. The chronic activation of the immune system can further damage the gut lining, creating a vicious cycle.
Furthermore, many conventionally grown gluten-containing grains are also heavily sprayed with glyphosate, a herbicide that has been shown to negatively impact the gut microbiome. This adds another layer of complexity for those seeking to improve their gut health. A gluten-free diet isn’t just about removing gluten; it’s about reducing overall inflammation and supporting the restoration of a healthy intestinal barrier. It’s important to remember, though, that simply eliminating gluten doesn’t automatically heal a leaky gut; a holistic approach is vital.
Building a Gluten-Free Plan for Gut Healing
A successful gluten-free plan for gut healing goes far beyond merely avoiding wheat bread and pasta. It requires mindful food choices focused on nourishing the gut lining, reducing inflammation, and supporting a diverse microbiome. This means prioritizing nutrient-dense foods, incorporating gut-healing superfoods, and addressing potential deficiencies. Start with a period of strict elimination to assess your body’s response, then gradually reintroduce gluten-free alternatives while monitoring for symptoms.
Focus on building your diet around naturally gluten-free whole foods like fruits, vegetables, lean proteins, healthy fats, and gluten-free grains (quinoa, brown rice, oats – certified gluten-free to avoid cross-contamination). Incorporate fermented foods such as kefir, sauerkraut, kimchi, and kombucha to promote a thriving microbiome. Bone broth is another excellent addition, providing collagen and amino acids that support gut lining repair. Hydration is also crucial; water helps flush toxins and supports healthy digestion. Avoid processed gluten-free products which can often be high in sugar and refined carbohydrates – these offer little nutritional value and can further disrupt the gut.
Crucially, a truly healing gluten-free plan isn’t about deprivation; it’s about abundance. It’s about discovering a wealth of delicious and nourishing alternatives that support your overall well-being. This often involves learning to cook more from scratch and experimenting with new recipes. Consider working with a registered dietitian or nutritionist specializing in gut health to create a personalized plan tailored to your specific needs and sensitivities.
Incorporating Gut-Healing Foods
Foods play an enormous role in repairing and maintaining the gut lining. Beyond just removing gluten, actively incorporating foods that support gut health is essential. – Collagen-rich foods: Bone broth, collagen peptides, or foods containing proline and glycine (found in animal proteins) can help rebuild damaged tissues in the gut lining. – Prebiotic foods: These feed beneficial bacteria in the gut. Examples include garlic, onions, leeks, asparagus, bananas, and apples. – Probiotic foods: As mentioned earlier, fermented foods are excellent sources of probiotics, which directly introduce beneficial bacteria to the gut.
Adding these types of food isn’t a one time fix but should be integrated into your diet long term for lasting benefits. Remember that dietary changes take time to show results; consistency is key. It’s also important to note that some individuals may experience histamine intolerance with fermented foods, so start slowly and monitor your body’s response.
Addressing Nutrient Deficiencies
A compromised gut lining often leads to malabsorption of essential nutrients. Gluten sensitivity or celiac disease can specifically impair the absorption of iron, calcium, vitamin D, folate, and B12. Even without a formal diagnosis, chronic inflammation caused by gluten can interfere with nutrient uptake. Therefore, identifying and addressing potential deficiencies is crucial for optimal gut healing.
Consider getting tested for common nutritional deficiencies through your healthcare provider. Supplementation may be necessary in some cases, but it’s generally best to obtain nutrients from whole food sources whenever possible. Focus on including foods rich in these essential vitamins and minerals in your diet. For example: – Iron: Red meat (if tolerated), spinach, lentils – combine with Vitamin C for better absorption. – Vitamin D: Fatty fish, egg yolks, fortified foods – consider supplementation during winter months. – B Vitamins: Leafy greens, eggs, poultry – a B-complex supplement may be helpful.
Managing Stress & Lifestyle Factors
Gut health isn’t solely dictated by diet; stress plays a significant role. Chronic stress can negatively impact the gut microbiome, increase intestinal permeability, and exacerbate inflammation. Implementing stress management techniques is therefore an integral part of any gut healing plan. – Mindfulness practices: Meditation, yoga, deep breathing exercises – even 10-15 minutes daily can make a difference. – Regular exercise: Physical activity releases endorphins which have mood-boosting effects and reduce stress. – Adequate sleep: Aim for 7-8 hours of quality sleep each night to allow your body to repair and regenerate.
Additionally, reducing exposure to toxins in everyday life (cleaning products, personal care items) can further support gut health. Prioritize organic foods whenever possible to minimize pesticide intake. Remember that healing the gut is a holistic process that requires addressing all aspects of lifestyle. It’s not just about what you don’t eat, but also about cultivating habits that promote overall well-being.