Fasting, an ancient practice rooted in various cultures for spiritual, religious, and health reasons, is experiencing a resurgence in popularity today. Beyond weight management, individuals are increasingly exploring fasting protocols for potential benefits ranging from improved metabolic health to enhanced cognitive function. However, the impact of fasting extends far beyond these commonly cited advantages; it significantly influences the intricate workings of our digestive system, specifically gut motility – the process by which food moves through the gastrointestinal tract. Understanding this interplay is crucial, as alterations in gut motility can profoundly affect overall wellbeing and dictate whether a fasting experience feels beneficial or disruptive.
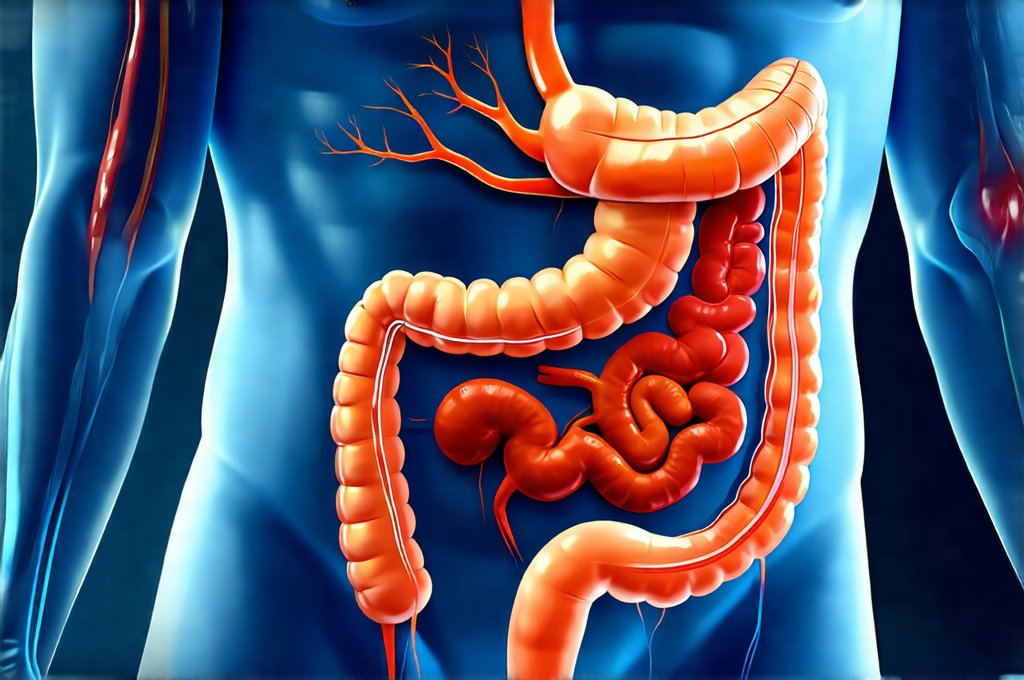
The human gut is far more than just a processing plant for food; it’s an ecosystem teeming with trillions of microorganisms – the gut microbiome – that play a vital role in immunity, nutrient absorption, mental health, and even disease prevention. Gut motility isn’t simply about speed; it encompasses the coordinated contractions of muscles along the digestive tract, ensuring efficient digestion, absorption, and elimination. Fasting introduces periods of both reduced intake and altered hormonal signals, which directly impact these processes. This can lead to changes in how quickly food moves through your system, how efficiently nutrients are absorbed, and ultimately, how comfortable you feel during a fast. A nuanced understanding is key because what works for one person’s gut may not work for another’s; individual responses vary greatly depending on factors like pre-existing conditions, dietary habits, and the type of fasting protocol employed. Considering how [your gut health] affects overall wellbeing can be helpful when starting a new diet plan.
The Interplay Between Fasting & Gut Motility: A Baseline Shift
Fasting fundamentally alters the digestive landscape. When we consistently provide our bodies with food, the gut is in a constant state of activity – peristalsis, the wave-like muscle contractions that propel food forward, are continuously engaged. This sustained activity leads to a certain baseline level of motility. However, when food intake ceases or drastically reduces during fasting, the digestive system undergoes a significant shift. The ‘digestive fire’ slows down; peristaltic movements become less frequent and less vigorous. This isn’t necessarily negative – it allows the gut time for essential housekeeping functions like cellular repair and microbiome modulation.
This slowdown is largely mediated by changes in hormonal regulation. Insulin levels drop during fasting, while glucagon (a hormone that helps release stored glucose) rises. These shifts impact the migrating motor complex (MMC), a series of strong contractions that sweep through the small intestine between meals, clearing out undigested food and bacteria. The MMC is typically suppressed when we eat, but it’s essential for maintaining gut health. Fasting promotes more regular and robust MMC activity because there’s no incoming food to interrupt it. This ‘gut cleaning’ effect is often cited as one of the benefits of fasting, though scientific research is still evolving in this area. You can also learn [how to keep your gut calm] during a busy schedule while adjusting to changes.
Crucially, the length of the fast impacts these changes. Intermittent fasting (IF), with shorter periods of restriction, may lead to more subtle shifts in motility than prolonged water-only fasts. Prolonged fasting can significantly reduce gastric emptying rates and intestinal transit time – meaning food takes longer to move through the system when reintroduced after a long period without intake. This is why refeeding syndrome, where rapid reintroduction of nutrients after starvation causes dangerous electrolyte imbalances, is a serious concern with extended fasts and highlights the need for careful planning and medical supervision.
Fasting Protocols & Their Unique Motility Effects
Different fasting protocols exert different levels of influence on gut motility. Intermittent fasting (IF), encompassing methods like 16/8 (eating within an 8-hour window, fasting for 16 hours) or 5:2 (normal eating five days a week, restricted calories two days), generally causes milder changes in motility compared to more restrictive approaches. The regular periods of eating allow the gut to maintain some level of activity and prevent extreme slowdowns. However, even IF can still promote MMC activity during fasting windows, aiding in gut cleaning and potentially improving digestive efficiency.
Extended fasts – those lasting 24 hours or longer – induce a more pronounced reduction in motility. During water-only fasts, for example, the stomach may empty slower than usual, and intestinal contractions become less frequent. This can result in decreased bowel movements and a feeling of fullness even without consuming food. The reintroduction of food after an extended fast requires careful consideration to avoid digestive distress. Starting with easily digestible foods in small portions is vital to allow the gut to gradually resume its normal function.
Furthermore, modified fasting approaches – such as incorporating bone broth or small amounts of healthy fats during a prolonged fast – can partially mitigate these motility changes. These additions provide some minimal input for the digestive system without fully disrupting the metabolic benefits of fasting. However, it’s important to remember that even small amounts of food can suppress MMC activity and alter hormonal signals. The ideal protocol will always depend on individual tolerance and goals. Understanding [how intermittent fasting affects hormone levels] is vital before starting a new diet plan.
Addressing Constipation During Fasting
Constipation is a common complaint during fasting, especially with longer fasts or in individuals prone to digestive issues. The reduced intake of fiber-rich foods and the slowing down of gut motility contribute to this issue. However, it’s important to distinguish between normal variations in bowel movements and true constipation. During a fast, fewer bowel movements are expected – the absence of significant food volume means there’s less waste to eliminate.
Here are some strategies that might help alleviate constipation during fasting:
- Hydration is Key: Drinking plenty of water throughout the day is crucial for softening stool and promoting gut motility. Aim for at least 8 glasses (64 ounces) per day, or more if you’re active.
- Gentle Movement: Light exercise, such as walking or yoga, can stimulate peristalsis and help move things along. Avoid strenuous activity that might put undue stress on the digestive system.
- Magnesium Supplementation (with caution): Magnesium citrate is a natural laxative that can help draw water into the intestines and soften stool. However, it’s important to consult with a healthcare professional before taking magnesium supplements, as they can interact with certain medications or exacerbate existing health conditions. Start with a low dose and monitor your response carefully.
Important Note: Avoid using harsh laxatives during fasting, as these can disrupt electrolyte balance and potentially lead to dehydration. If constipation persists despite these measures, it’s essential to consult with a healthcare professional.
The Role of the Gut Microbiome in Fasting Response
The gut microbiome plays an integral role in how we respond to fasting. As mentioned earlier, fasting promotes MMC activity, which can help clear out bacteria from the small intestine. This process can lead to shifts in the composition of the gut microbiome, potentially reducing populations of harmful bacteria and promoting the growth of beneficial ones. However, the specific changes that occur are complex and depend on individual factors like pre-existing microbiome diversity and dietary habits.
Fasting also influences the production of short-chain fatty acids (SCFAs) – metabolites produced by gut bacteria when they ferment fiber. While fiber intake is limited during fasting, SCFAs can still be produced from endogenous sources (e.g., breakdown of intestinal cells) or from small amounts of resistant starch that may remain in the gut. SCFAs have numerous health benefits, including strengthening the gut barrier and reducing inflammation.
Furthermore, emerging research suggests that specific microbial populations may thrive during fasting, contributing to its beneficial effects. For example, certain bacteria are known to increase their production of butyrate, a SCFA with potent anti-inflammatory properties, when glucose availability is limited – as it is during fasting. Understanding the complex interplay between fasting and the gut microbiome is an area of ongoing research and may lead to more personalized fasting strategies in the future. Recognizing [how your gut health affects reflux frequency] can help you better understand your body’s response.
Reintroducing Food: A Gradual Approach to Restore Motility
Reintroducing food after a fast requires careful planning to avoid digestive upset. As discussed, gut motility slows down during fasting, so the digestive system needs time to readjust when food is reintroduced. The key principle is gradualism. Avoid overwhelming the system with large meals or complex foods immediately after breaking the fast.
Here’s a suggested approach for refeeding:
- Start Small: Begin with easily digestible foods in small portions, such as bone broth, cooked vegetables (e.g., steamed carrots or zucchini), or plain yogurt.
- Prioritize Easily Digested Foods: Focus on foods that are gentle on the digestive system and less likely to cause bloating or discomfort. Examples include: – Soups & Broths – Fermented Foods (yogurt, kefir) – Cooked Fruits (applesauce) – Lean Proteins (fish, chicken)
- Gradually Increase Portion Sizes & Complexity: Over several days, gradually increase the portion sizes and introduce more complex foods like whole grains, lean proteins, and healthy fats. Pay attention to your body’s signals and adjust accordingly.
It’s also essential to chew food thoroughly and eat mindfully to aid digestion. Avoid combining large amounts of fat and carbohydrates in the same meal, as this can be challenging for a digestive system that is still recovering from fasting. If you experience any digestive discomfort during refeeding, reduce your portion sizes or revert to simpler foods until symptoms subside. Considering [how stress affects your ability to burn fat] may help with overall wellbeing.