Fasting, an ancient practice with roots in various cultures and spiritual traditions, is experiencing a resurgence in popularity driven by potential health benefits ranging from weight management to improved cellular repair. While often associated with dietary changes, the impact of fasting extends far beyond simply restricting food intake; it profoundly affects numerous physiological processes within the body. One area garnering increasing attention is its influence on hemostasis, the intricate system responsible for blood clotting and maintaining healthy circulation. Understanding how fasting interacts with these vital functions is crucial, particularly given that both excessive clotting (thrombosis) and insufficient clotting (hemorrhage) can pose serious health risks. It’s important to note that individual responses to fasting vary considerably based on factors like pre-existing conditions, duration of the fast, and overall health status.
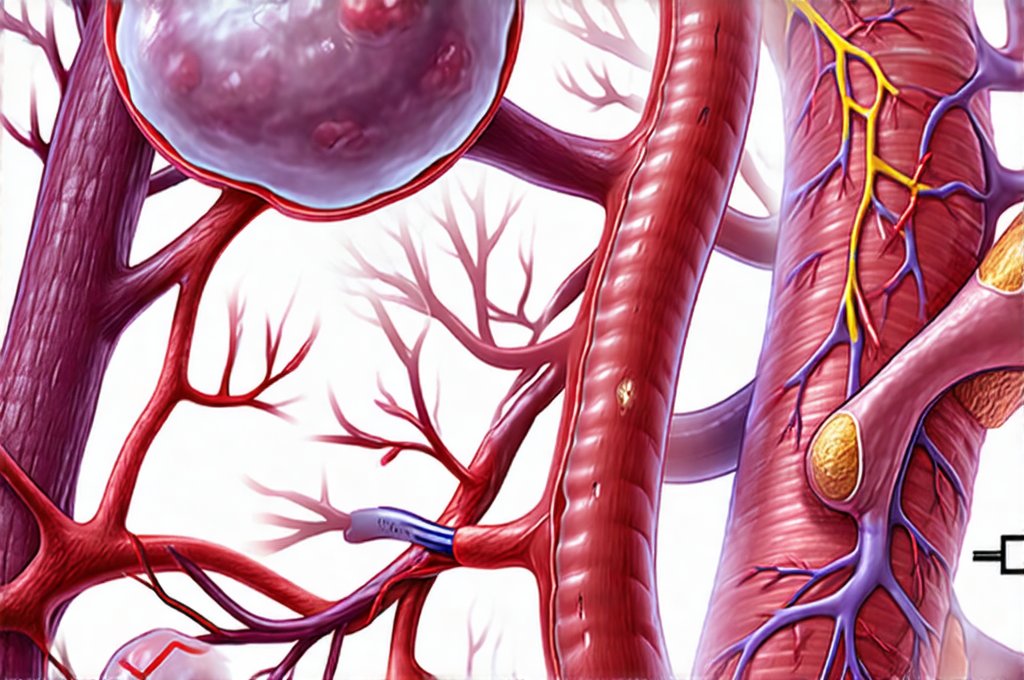
The body’s response to prolonged periods without food is multifaceted. Initially, it utilizes glycogen stores for energy – readily available glucose from the liver and muscles. As these deplete, the metabolic shift transitions towards ketogenesis, where fat is broken down into ketones as an alternative fuel source. This metabolic flexibility isn’t simply a matter of finding new energy; it triggers hormonal changes affecting everything from insulin sensitivity to inflammation levels. These shifts directly impact blood viscosity, platelet activity, and endothelial function – all key players in the clotting cascade and circulatory health. Therefore, assessing the effects of fasting on circulation and coagulation requires a nuanced understanding of these interconnected systems. Understanding how fasting impacts metabolism can help you prepare for changes in your body.
Fasting and Blood Viscosity/Circulation
Blood viscosity, or thickness, significantly influences how easily blood flows through vessels. Higher viscosity increases resistance, potentially leading to reduced oxygen delivery and increased cardiovascular strain. Dehydration exacerbates this issue, but fasting itself also plays a role. During fasting, the body mobilizes water stores as part of metabolic processes – including ketogenesis – which can contribute to mild dehydration if adequate fluid intake isn’t maintained. However, paradoxically, despite potential for dehydration, some studies suggest that prolonged fasting might reduce blood viscosity in certain individuals. This is thought to be linked to changes in protein concentrations and red blood cell composition during metabolic adaptation.
The effect on circulation is closely tied to these viscosity changes. Improved circulation means better nutrient delivery, waste removal, and overall cellular function. Fasting, through its impact on inflammation and endothelial function (the inner lining of blood vessels), can potentially enhance vascular health over time. Endothelial dysfunction is a major contributor to cardiovascular disease, and interventions that improve endothelial function are highly valued. However, it’s crucial to understand that the relationship isn’t linear; very rapid or extreme fasting could initially stress the circulatory system as the body adapts to new energy demands.
Furthermore, hormonal changes during fasting – specifically decreases in insulin and increases in growth hormone – can influence blood vessel tone and dilation. Insulin resistance is often associated with impaired endothelial function, so reducing insulin levels through fasting may contribute to improved vascular health. This highlights the complex interplay between metabolic hormones, blood viscosity, and overall circulatory performance. It’s also important to emphasize that maintaining proper hydration during a fast is paramount to supporting healthy circulation and preventing unwanted increases in blood viscosity. For those with concerns about both diabetes and high blood pressure, how to eat can be an important consideration.
Impact on Platelet Aggregation
Platelets are essential for initiating blood clotting; they adhere to damaged vessel walls and begin the process of forming a clot. Platelet aggregation – the clumping together of platelets – is a critical step, but excessive aggregation can lead to dangerous thrombus formation. Research suggests that fasting may influence platelet activity in several ways. Some studies have shown a decrease in platelet reactivity during prolonged water-only fasts, potentially reducing the risk of unwanted clotting. This reduction might be linked to changes in inflammatory markers and improved endothelial function.
However, it’s not universally observed, and the effects can vary depending on the type of fasting (intermittent vs. prolonged), individual health status, and other factors. For example, individuals with pre-existing cardiovascular conditions or those taking blood thinners should exercise extreme caution when considering fasting, as alterations in platelet function could potentially increase bleeding risk. Moreover, refeeding after a fast can sometimes temporarily increase platelet reactivity as the body readjusts to food intake – this is known as the “refeeding syndrome” and needs careful consideration.
The mechanisms behind these changes are still being investigated. It’s believed that fasting-induced reductions in inflammation may play a role, as inflammatory cytokines often promote platelet activation. Additionally, ketones produced during ketogenesis might have antiplatelet effects, though more research is needed to confirm this. Ultimately, the impact on platelet aggregation appears to be a dynamic process influenced by multiple factors and requires careful consideration within an individual’s health context.
The Role of Endothelial Function
The endothelium isn’t just a passive barrier; it actively regulates blood flow, prevents clot formation, and influences vascular tone. Endothelial dysfunction is a hallmark of many chronic diseases, including cardiovascular disease, diabetes, and obesity. Fasting can positively impact endothelial function through several mechanisms. As previously mentioned, reducing insulin resistance improves endothelial health, as high insulin levels are often associated with endothelial damage.
Furthermore, fasting promotes autophagy – the cellular process of “self-cleaning” where damaged components are removed – which can help clear out dysfunctional cells within the endothelium. This cellular renewal contributes to a healthier and more resilient vascular lining. Additionally, the reduction in oxidative stress that often accompanies fasting helps protect the endothelium from damage caused by free radicals.
However, it’s crucial to avoid extremes. Rapid or prolonged dehydration associated with improper fasting can worsen endothelial function. Therefore, maintaining adequate hydration and electrolyte balance is essential for supporting vascular health during a fast. The interplay between fasting, endothelial function, and overall circulatory health highlights the importance of a holistic approach that considers both dietary restriction and supportive lifestyle factors. If you are looking to support your circulation through diet, consider herbs and spices as well!
Considerations for Individuals on Blood Thinners
Individuals taking anticoagulant or antiplatelet medications (blood thinners) need to be particularly cautious when considering fasting. These medications are designed to reduce blood clotting, and combining them with the potential anticoagulant effects of fasting could significantly increase the risk of bleeding. It is absolutely essential to consult with a healthcare professional before undertaking any fast if you are on blood-thinning medication.
Adjusting medication dosages during fasting may be necessary, but this should only be done under strict medical supervision. Monitoring blood clotting parameters (e.g., INR for warfarin) is crucial to ensure that the anticoagulation level remains within a safe range. Furthermore, recognizing signs of excessive bleeding – such as prolonged bruising, nosebleeds, or bloody stools – and seeking immediate medical attention are vital if any occur during fasting.
It’s also important to remember that refeeding after a fast can alter medication effectiveness; close monitoring is needed during the refeeding period to prevent both bleeding and clotting risks. The interaction between fasting and blood-thinning medications is complex, and personalized guidance from a qualified healthcare provider is paramount to ensure safety and minimize potential complications.
It’s important to reiterate that this information isn’t intended as medical advice. Fasting can have profound effects on the body, including its clotting mechanisms and circulation, but individual responses vary greatly. Any decisions regarding fasting should be made in consultation with a qualified healthcare professional who can assess your specific health status and provide tailored guidance. You might also want to consider how blood pressure changes as you age.