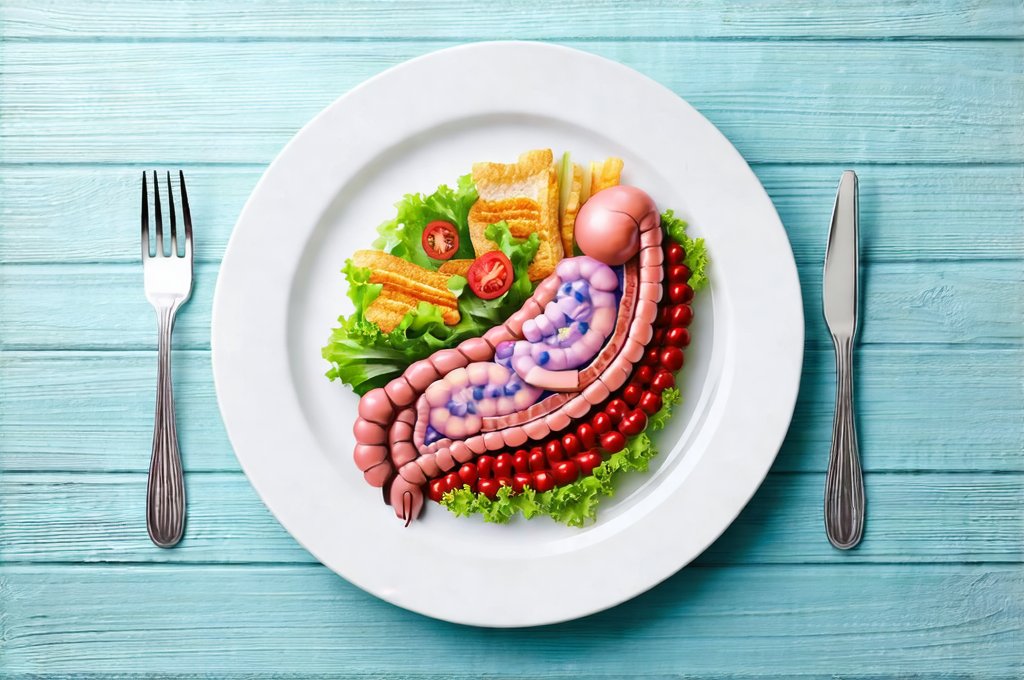
The gut – often referred to as our “second brain” – plays an incredibly vital role in overall health far beyond simply digesting food. It impacts everything from immunity and mental wellbeing to nutrient absorption and hormone regulation. When the delicate balance within the intestinal environment is disrupted, leading to conditions like leaky gut, Inflammatory Bowel Disease (IBD), or even general digestive distress, a focused dietary approach can be one of the most powerful tools for healing. Many factors contribute to this imbalance – stress, poor diet choices, overuse of antibiotics, and environmental toxins are just a few examples. Recognizing that food is medicine is the first step toward restoring gut health, but knowing which foods to prioritize (and which to avoid) can feel overwhelming.
This article will explore how a carefully constructed meal plan, prioritizing nutrient density and minimizing inflammatory triggers, can actively support intestinal healing. It’s important to understand this isn’t about restrictive dieting; it’s about nourishing your body with the building blocks it needs to repair and rebuild the gut lining. We will delve into specific food choices, dietary strategies, and practical tips for implementing a healing diet that feels sustainable and empowers you to take control of your digestive wellbeing. This is not intended as medical advice, but rather a guide to understanding how thoughtful nutrition can be integrated into a holistic approach to gut health in conjunction with professional healthcare guidance.
Foundations of an Intestinal Healing Diet
The cornerstone of any intestinal healing diet is reducing inflammation and providing the necessary nutrients for tissue repair. A key principle is elimination – temporarily removing foods known to irritate the gut, then strategically reintroducing them to identify individual sensitivities. This process often involves identifying food triggers which vary significantly from person to person. Focusing on whole, unprocessed foods is paramount. Think vibrant fruits and vegetables, lean proteins, healthy fats, and fermented foods that contribute to a diverse microbiome. Equally important is hydration – adequate water intake supports optimal digestion and nutrient absorption.
A typical healing diet often emphasizes easily digestible foods while minimizing complex carbohydrates and potentially irritating substances. This isn’t necessarily about cutting out entire food groups permanently; it’s more about providing the gut with a period of rest and recovery. Many people find success with diets inspired by principles like the Specific Carbohydrate Diet (SCD) or Low-FODMAP diet, though these should be implemented under professional guidance. The goal is to reduce the workload on the digestive system, allowing it time to heal and rebuild its protective barrier. Prioritizing nutrient density ensures that every bite contributes to overall health and supports the body’s natural healing processes.
It’s also crucial to address potential deficiencies. Chronic gut issues often lead to malabsorption of essential vitamins and minerals. Therefore, incorporating foods rich in nutrients like Vitamin D, zinc, magnesium, and omega-3 fatty acids can be incredibly beneficial. Supplementation might be necessary in some cases, but it’s always best determined by a healthcare professional based on individual needs and testing. Remember that intestinal healing is a journey, not a destination. Consistency and patience are key to seeing lasting results.
Building Blocks: Core Food Groups for Gut Health
- Bone Broth: Rich in collagen and amino acids, bone broth helps rebuild the gut lining and reduces inflammation. Homemade is best, but high-quality store-bought options are available.
- Fermented Foods: Yogurt (dairy or non-dairy), kefir, sauerkraut, kimchi, and kombucha introduce beneficial bacteria to the gut microbiome, promoting a healthy balance.
- Lean Proteins: Easily digestible proteins like fish, poultry, and eggs provide essential amino acids for tissue repair without overburdening the digestive system.
- Healthy Fats: Avocado, olive oil, coconut oil, and fatty fish (salmon, mackerel) support overall health and reduce inflammation.
- Low-Starch Vegetables: Leafy greens, broccoli, cauliflower, carrots, and zucchini are packed with vitamins and minerals and are generally well-tolerated by sensitive guts.
The selection of protein sources is important. Red meat can be harder to digest for some individuals with gut issues, so opting for smaller portions or choosing leaner cuts might be beneficial. Similarly, dairy can be problematic for many, leading to inflammation. Experimenting with alternatives like almond milk, coconut yogurt, or lactose-free options can help determine individual tolerance levels.
The importance of fiber cannot be overstated, but the type of fiber matters. Soluble fiber found in oats and sweet potatoes is often better tolerated than insoluble fiber from wheat bran during initial healing phases. Gradually reintroducing more complex fibers as gut health improves is a good approach. This allows the microbiome to adapt and thrive without causing excessive discomfort.
Hydration & Digestive Support
Proper hydration is absolutely fundamental to intestinal healing. Water helps move food through the digestive tract, prevents constipation, and supports nutrient absorption. Aim for at least eight glasses of water per day, or more if you are physically active or live in a hot climate. Herbal teas, such as ginger or chamomile, can also contribute to hydration while offering additional calming benefits. Avoid sugary drinks and excessive caffeine, which can irritate the gut.
Beyond water, certain beverages can actively support digestion. Ginger tea is known for its anti-inflammatory properties and helps relieve nausea. Peppermint tea can soothe digestive muscles and reduce bloating. Bone broth, as previously mentioned, provides crucial nutrients for healing. Conversely, alcohol and carbonated beverages should be minimized or avoided altogether during the initial stages of gut healing as they can exacerbate symptoms.
Digestive enzymes can also be a valuable addition to your routine, particularly if you struggle with food intolerances or malabsorption. These supplements help break down food into smaller, more easily digestible components, reducing strain on the digestive system. Probiotic supplementation might also be considered, but it’s important to choose a high-quality probiotic with diverse strains and consult with a healthcare professional to determine the appropriate dosage and form.
Meal Planning & Practical Implementation
Creating a meal plan is essential for staying consistent with an intestinal healing diet. Start by identifying foods you know cause discomfort and eliminate them temporarily. Then, focus on building meals around core food groups – lean proteins, healthy fats, low-starch vegetables, and fermented foods. Prepare meals in advance whenever possible to avoid impulsive choices that might derail your progress.
Here’s a sample meal plan for someone starting their intestinal healing journey:
1. Breakfast: Oatmeal with berries and almond milk, or scrambled eggs with avocado.
2. Lunch: Grilled chicken salad with mixed greens, olive oil vinaigrette, and avocado.
3. Dinner: Baked salmon with roasted broccoli and sweet potato.
4. Snacks: Bone broth, plain yogurt (dairy or non-dairy), or a handful of almonds.
Remember to listen to your body and adjust the plan based on your individual needs and tolerances. Food journaling can be an incredibly helpful tool for identifying trigger foods and tracking progress. Don’t be afraid to experiment with different recipes and variations within the framework of the healing diet. The goal is to find a sustainable approach that nourishes your body and supports long-term gut health, not to restrict yourself unnecessarily. It is also important to remember that seeking guidance from a registered dietitian or healthcare professional specializing in gut health can provide personalized support and ensure you’re meeting your nutritional needs effectively.