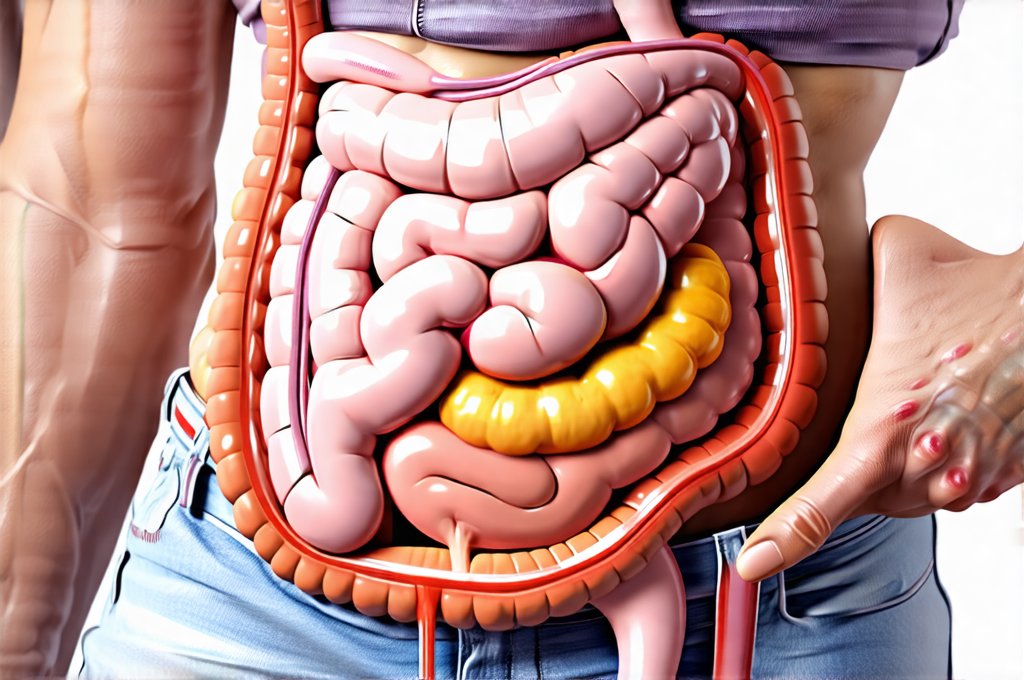
Polycystic Ovary Syndrome (PCOS) is a complex endocrine disorder affecting millions worldwide, often characterized by irregular periods, excess androgen levels, and/or polycystic ovaries. However, the story doesn’t end there. Increasingly, research highlights a strong connection between PCOS and the gut microbiome – the trillions of bacteria, fungi, viruses, and other microorganisms residing in our digestive tract. This isn’t merely a correlation; it suggests a bidirectional relationship where imbalances in the gut can contribute to PCOS symptoms, and conversely, PCOS itself can disrupt the delicate ecosystem within us. Understanding this interplay is crucial for developing more holistic and effective management strategies beyond traditional hormonal treatments.
The conventional approach to PCOS often centers around managing individual symptoms like irregular cycles or acne. While necessary, it frequently overlooks the foundational health of the gut. A compromised gut microbiome can lead to chronic low-grade inflammation, insulin resistance (a hallmark of PCOS), and altered hormone metabolism – all contributing factors that exacerbate the condition. Restoring gut balance isn’t a quick fix, but rather an integral component of long-term wellness for those living with PCOS, offering potential benefits in symptom management and overall quality of life. This article will explore the intricate link between PCOS and gut health, outlining practical steps toward achieving microbiome harmony.
The Gut-PCOS Connection: A Deeper Dive
The relationship between the gut microbiome and PCOS isn’t a new discovery but recent advancements in research are painting a much clearer picture of how this connection works. Studies have consistently shown distinct differences in the gut microbial composition of individuals with PCOS compared to those without. Specifically, there’s often reduced diversity – meaning fewer different types of beneficial bacteria – and an increase in certain bacterial species associated with inflammation. This imbalance can disrupt the intestinal barrier, leading to “leaky gut” syndrome where undigested food particles and toxins enter the bloodstream, triggering an immune response and further fueling inflammation.
This systemic inflammation then impacts hormonal balance. For instance, it can interfere with ovarian function, worsen insulin resistance (making it harder for cells to respond to insulin and potentially leading to higher blood sugar levels), and increase androgen production – all key features of PCOS. Moreover, the gut microbiome plays a role in estrogen metabolism. Certain bacteria produce an enzyme called beta-glucuronidase which can reactivate estrogen in the gut, potentially contributing to estrogen dominance, another common issue in some presentations of PCOS. The influence extends even further; the gut influences neurotransmitter production, impacting mood and potentially contributing to the anxiety and depression sometimes associated with living with a chronic condition like PCOS.
It’s important to remember that this isn’t a one-way street. PCOS itself can create conditions within the body that negatively impact the gut microbiome. Factors such as insulin resistance, inflammation, and dietary choices often associated with PCOS (highly processed foods, sugary drinks) can further disrupt the gut ecosystem, creating a vicious cycle. This underscores the need for an integrated approach to management focusing on both symptom relief and gut health restoration.
Dietary Strategies for Gut Healing in PCOS
Diet is arguably the most powerful tool we have when it comes to influencing our gut microbiome. It’s not about restrictive dieting but rather making informed choices that nourish beneficial bacteria and minimize inflammation. Here’s a breakdown of key dietary strategies:
- Prioritize Fiber: Fiber acts as “food” for beneficial gut bacteria, promoting their growth and diversity. Aim for 25-35 grams per day from sources like vegetables (broccoli, spinach, Brussels sprouts), fruits (berries, apples, pears), legumes (beans, lentils, chickpeas), and whole grains (oats, quinoa, brown rice). Introducing fiber gradually is crucial to avoid digestive discomfort.
- Embrace Fermented Foods: These foods are naturally rich in probiotics – live microorganisms that can colonize the gut and improve microbial balance. Examples include yogurt (choose plain, unsweetened varieties with live cultures), kefir, sauerkraut, kimchi, kombucha, and miso.
- Reduce Sugar & Processed Foods: Excessive sugar feeds harmful bacteria and promotes inflammation. Minimize intake of refined sugars, sugary drinks, processed snacks, and highly processed foods that lack nutritional value.
Beyond specific food choices, mindful eating is also important. Taking the time to chew your food thoroughly aids digestion and allows enzymes to work more effectively. Staying hydrated is essential for gut health as water helps move waste through the digestive system. Consider an elimination diet under the guidance of a healthcare professional to identify potential food sensitivities that might be contributing to inflammation. Affordable meal plans can also assist with this process.
The Role of Prebiotics & Probiotics
Prebiotics and probiotics are often talked about together, but they play distinct roles in supporting gut health. Probiotics are live microorganisms that provide a direct boost to the gut microbiome, while prebiotics are types of fiber that feed existing beneficial bacteria. Think of prebiotics as fertilizer for your good bacteria.
- Probiotic Supplements: While food sources are ideal, probiotic supplements can be helpful, especially during periods of dysbiosis (microbial imbalance). However, it’s crucial to choose a high-quality supplement with diverse strains and CFUs (colony forming units) appropriate for individual needs. Consider consulting with a healthcare professional to determine the best strain combination for you.
- Prebiotic Rich Foods: Include foods like onions, garlic, leeks, asparagus, bananas, oats, apples, and chicory root in your diet to nourish beneficial bacteria.
- Synergistic Approach: Combining prebiotics and probiotics can create a synergistic effect, enhancing the growth and activity of beneficial microbes. This is known as synbiotic therapy.
It’s important to note that not all probiotic supplements are created equal. Some strains may be more effective for specific conditions than others. Also, introducing too many probiotics at once can sometimes cause temporary digestive upset. Starting with a low dose and gradually increasing it over time is generally recommended. You might find benefits from a gut balance plan.
Stress Management & Gut Health
The gut-brain axis – the bidirectional communication pathway between the gut microbiome and the brain – highlights the profound impact of stress on gut health, and vice versa. Chronic stress can disrupt the gut microbiome, leading to inflammation and impaired digestion. In turn, an imbalanced gut can contribute to anxiety and mood disorders.
- Stress Reduction Techniques: Incorporate stress-reducing practices into your daily routine, such as yoga, meditation, deep breathing exercises, spending time in nature, or engaging in hobbies you enjoy.
- Prioritize Sleep: Adequate sleep is essential for both physical and mental well-being, including gut health. Aim for 7-9 hours of quality sleep per night.
- Mindful Movement: Regular exercise can help reduce stress and improve gut motility (the movement of food through the digestive tract). Choose activities you enjoy and find sustainable ways to incorporate them into your lifestyle.
Addressing underlying stressors is key to long-term gut health and overall well-being in PCOS management. This might involve therapy, counseling, or other forms of support to address emotional challenges and develop coping mechanisms. It’s a holistic approach that acknowledges the interconnectedness of mind, body, and gut. Emotional eating plans can be very helpful here.
It’s vital to remember that this information is for general knowledge and informational purposes only, and does not constitute medical advice. Always consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.