Silent reflux, also known as laryngopharyngeal reflux (LPR), is often called the “silent” condition because its symptoms differ significantly from typical heartburn associated with gastroesophageal reflux disease (GERD). While GERD usually presents with a burning sensation in the chest, silent reflux frequently manifests with seemingly unrelated issues like chronic cough, hoarseness, or persistent throat clearing. This difference makes it challenging to diagnose and often leads to misdiagnosis or delayed treatment, impacting quality of life for those affected. Understanding what sets LPR apart is the first step toward effectively managing its symptoms and finding relief.
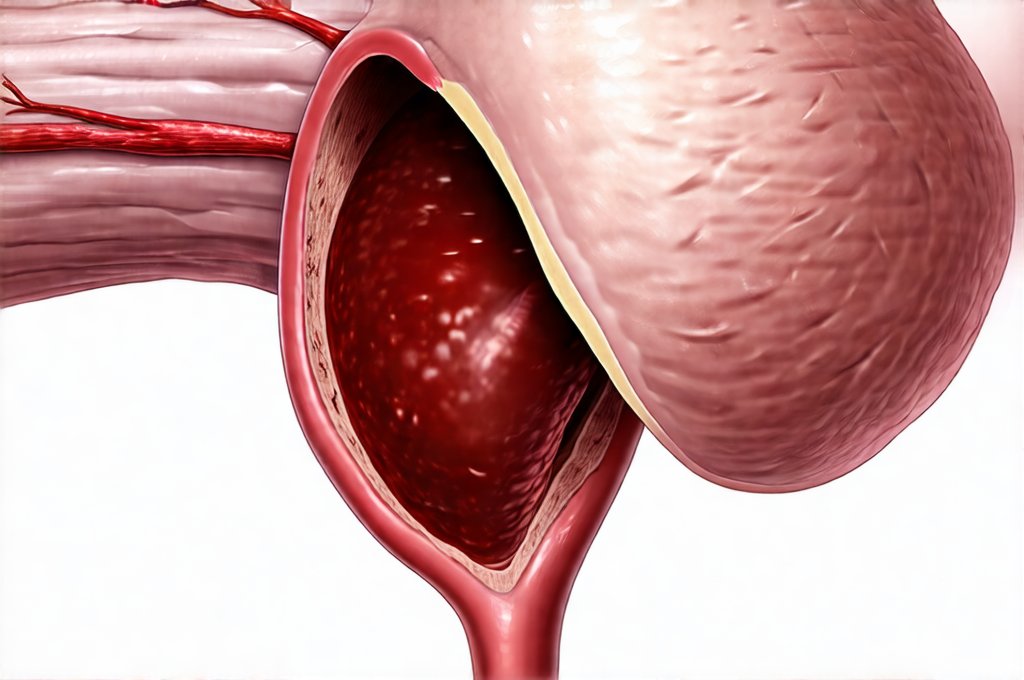
Unlike GERD where stomach acid predominantly travels up into the esophagus causing inflammation there, in silent reflux, gastric contents – including acid, pepsin (a digestive enzyme), and bile acids – travel higher up, reaching the larynx (voice box) and pharynx (throat). This ‘refluxate’ is incredibly irritating to these delicate tissues, even in small amounts. Many individuals experiencing LPR don’t experience typical heartburn symptoms at all, or if they do, it may be very mild and infrequent, further contributing to the difficulty in recognizing the condition. It’s crucial to understand that the absence of classic GERD symptoms doesn’t necessarily mean reflux isn’t occurring; it simply means it’s manifesting differently.
Understanding The Symptoms Of Silent Reflux
The insidious nature of silent reflux stems from its diverse and often subtle symptoms, making diagnosis challenging. Many people attribute these symptoms to allergies, asthma, or even postnasal drip, leading to a prolonged search for the root cause. Identifying LPR requires looking beyond the typical heartburn picture and recognizing patterns in seemingly unrelated complaints. Common indicators include a persistent cough, particularly at night or after meals; a sensation of something stuck in the throat (globus sensation); frequent throat clearing; hoarseness or changes in voice quality; chronic sore throat without infection; and even ear pain. It’s important to note that these symptoms can fluctuate, appearing more pronounced during periods of stress or after consuming trigger foods.
The reason for this atypical presentation lies within the sensitivity of the upper aerodigestive tract. The esophagus has a protective lining capable of tolerating some acid exposure. However, the larynx and pharynx are much more vulnerable to damage from even small amounts of refluxate. This means that symptoms develop not because of strong acidic burns, but rather from constant irritation and inflammation caused by the pepsin and other components in gastric contents. Furthermore, this chronic irritation can lead to changes in the vocal cords or throat tissues over time, potentially causing long-term complications if left untreated.
The diagnostic process often involves a detailed medical history, physical examination of the throat, and sometimes specialized tests like impedance pH monitoring. This test measures both acid and non-acid reflux events, providing a more accurate picture than traditional pH monitoring used for GERD. It is also important to rule out other potential causes of these symptoms through appropriate investigations. Recognizing the constellation of symptoms is vital in prompting further evaluation and ultimately leading to an accurate diagnosis.
Identifying Triggers And Lifestyle Modifications
Managing silent reflux often begins with identifying personal triggers – foods, habits, or situations that exacerbate symptoms. There isn’t a one-size-fits-all list, as individual sensitivities vary considerably. However, some common culprits include: caffeine; alcohol; chocolate; mint; spicy foods; fatty foods; carbonated beverages; citrus fruits and juices; and tomato-based products. Keeping a food diary can be incredibly helpful in pinpointing which items worsen your symptoms. Beyond dietary triggers, lifestyle factors also play a significant role.
One of the most effective strategies for managing LPR is to adopt several key lifestyle modifications. These include: elevating the head of your bed by 6-8 inches (using blocks or a wedge pillow) to help prevent reflux during sleep; avoiding eating within 2-3 hours of bedtime; losing weight if overweight or obese, as excess abdominal pressure can contribute to reflux; and quitting smoking, as it weakens the lower esophageal sphincter. Eating smaller, more frequent meals instead of large ones can also reduce the risk of reflux. Practicing stress management techniques such as yoga, meditation, or deep breathing exercises can further help minimize symptoms.
These modifications aren’t a cure-all, but they form the foundation of LPR management and often significantly alleviate symptoms for many individuals. It’s about creating sustainable habits that reduce the frequency and severity of reflux events. Remember, consistency is key – even small changes implemented consistently over time can make a substantial difference in your overall well-being.
The Role Of Dietary Changes
Dietary adjustments are paramount in minimizing silent reflux symptoms. Beyond avoiding obvious triggers like caffeine and spicy foods, focusing on anti-inflammatory foods can provide additional benefits. Incorporating foods rich in omega-3 fatty acids (salmon, flaxseeds, walnuts) and antioxidants (berries, leafy greens) can help soothe inflammation in the throat and larynx. Hydration is also crucial – drinking plenty of water helps dilute stomach acid and keeps the digestive system functioning optimally.
A helpful approach to dietary management involves a process of elimination. Start by removing common triggers from your diet for several weeks and then gradually reintroduce them one at a time, carefully monitoring your symptoms after each addition. This allows you to identify specific sensitivities that might be contributing to your reflux. It’s also important to avoid overeating and to chew food thoroughly, aiding digestion and reducing the likelihood of acid reflux.
Consider consulting with a registered dietitian or nutritionist who can help you develop a personalized dietary plan tailored to your individual needs and preferences. They can provide guidance on creating balanced meals that minimize triggers while ensuring adequate nutritional intake. Remember: dietary changes are not about deprivation but about making informed choices that support your health and well-being.
Medication Options & Their Limitations
While lifestyle modifications are often the first line of defense, medication may be necessary for some individuals to manage their silent reflux symptoms effectively. Over-the-counter antacids can provide temporary relief from mild symptoms, but they don’t address the underlying cause of the reflux. Proton pump inhibitors (PPIs) and H2 receptor antagonists are medications commonly used to reduce stomach acid production. However, their effectiveness in LPR is often debated because the damage isn’t always caused by acid, but rather by other components of refluxate like pepsin.
Furthermore, long-term use of PPIs can have potential side effects, including nutrient deficiencies and increased risk of infections. Therefore, medication should be used judiciously under the guidance of a healthcare professional. Alginates are another option; these form a raft on top of stomach contents to prevent reflux into the esophagus and throat, offering targeted relief for some individuals.
It’s critical to understand that medications are typically used as an adjunct to lifestyle modifications, not as a replacement. The goal should be to minimize medication use over time by addressing underlying triggers and adopting healthy habits. Regular follow-up with your doctor is essential to monitor the effectiveness of treatment and adjust it as needed.
When To Seek Further Medical Evaluation
Recognizing when to seek further medical evaluation is crucial for effective management of silent reflux. If lifestyle modifications and over-the-counter medications aren’t providing adequate relief, or if symptoms are worsening despite these efforts, it’s time to consult a healthcare professional – preferably an otolaryngologist (ENT doctor) specializing in voice and swallowing disorders. Persistent hoarseness that doesn’t improve with rest; difficulty swallowing; chronic throat pain; or any changes in your voice should prompt immediate attention.
A thorough evaluation may involve specialized tests such as laryngoscopy (visual examination of the larynx), impedance pH monitoring, and esophageal manometry (measuring pressure within the esophagus). These tests help determine the extent of reflux and identify any underlying issues contributing to it. In some cases, further investigations might be needed to rule out other conditions that could mimic LPR symptoms.
Don’t hesitate to advocate for your health and seek a second opinion if you feel your concerns aren’t being adequately addressed. Early diagnosis and appropriate treatment can prevent long-term complications and significantly improve your quality of life. Remember: proactive management is key to navigating this often challenging condition.